This All-Female Practice Is Transforming Breast Cancer Treatment and Surgery

When Christie Miller, creator of the Christie Crushed Cancer blog, first received her breast cancer diagnosis, she consulted with—and promptly fired—three male surgeons. She felt as if her health and cosmetic concerns were being diminished due to implicit gender biases, a sentiment shared by many other breast cancer patients who have been told that what they want is impractical, impossible, or simply doesn’t matter by the very people tasked with keeping them healthy and alive.
It’s what Miller describes as “a standard of scare instead of a standard of care.” When her primary care doctor finally referred her to the Cassileth Plastic Surgery and Bedford Breast Center in Los Angeles, she felt something shift. “I knew from the moment I walked in that I was in the right place,” she says.
Cassileth Plastic Surgery and the Bedford Breast Center is the first plastic surgery and breast oncological surgery joint practice in the United States to work in tandem with one another to find the best cure and method of care. This unique cosmetic approach revolutionizes the way breast cancer patients are treated throughout their journeys.
Lisa Cassileth, the founder of the joint practice, speaks from experience. “The more you ask, the more you find that many women have had unpleasant experiences, from the biopsy performed by the silent radiologist, the lumpectomy performed by the surgeon who placed the scar right across the chest, to the pain or deformity of a mastectomy reconstruction,” she says.
Breast cancer is unfortunately very common, affecting about one out of eight women in the United States. Patients who experience early-stage breast cancer often have to choose between treatment options that do not always create the best cosmetic outcome: a mastectomy, where the entire breast is removed; or a breast-preserving procedure, where the surgeon removes cancerous masses and nearby tissue. But it doesn’t have to be that way.
“All the other surgeons told me, ‘You’re going to need a mastectomy if you don’t do chemo and radiation,’” Miller explains. “Instead Dr. Heather said, ‘We can totally do a lumpectomy,’ and then Dr. Miller comes in and says, ‘And we can lift them too.’ So now I get to be perky at 57.”
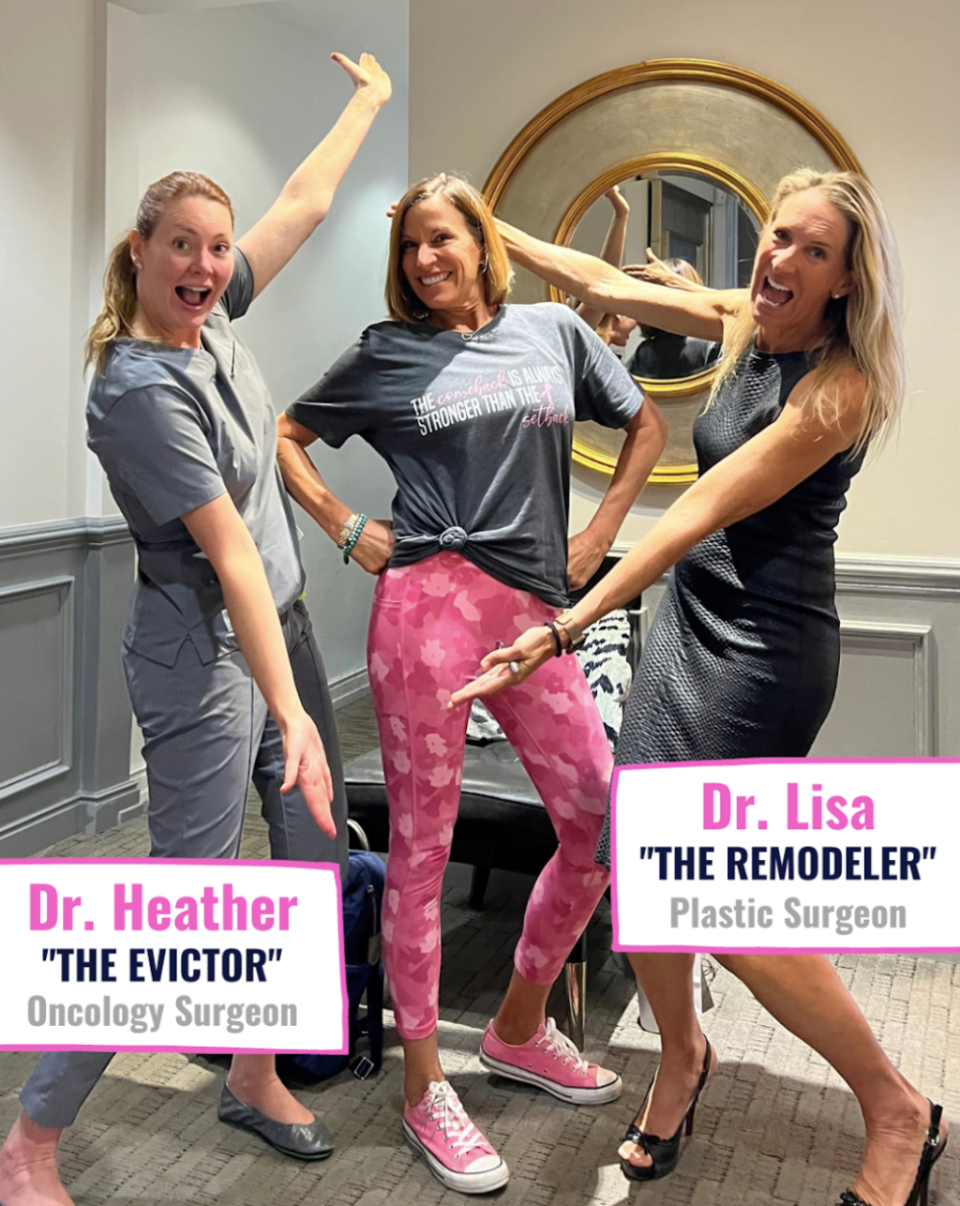
Heather Richardson, a breast surgeon at the Bedford Breast Center, promotes a customized plan for each patient rather than taking what she calls “a cookie-cutter approach to disease in women.” This includes medical innovations like novel mastectomy techniques that push the envelope and give women more chances to fight breast cancer, while also creating a cosmetic outcome that makes them feel beautiful.
“Many people have the mistaken impression that breast disease moves forward in a very linear fashion, that it starts as a small speck and slowly gets larger and larger, and if it’s caught in that timeline, ‘early’ enough, then a smaller surgery with less tissue removal is possible and mastectomy is less likely,” Richardson says. “Unfortunately, breast disease is actually a much more complicated situation.”
The center uses surgical advancements pioneered by women, like nerve grafts, to treat their patients. Cassileth and her colleagues are among the physicians spearheading these new technologies.
“In 2021, our surgical team was the first in Los Angeles to perform nerve grafts during mastectomy, allowing the breast to be reinnervated for sensation after mastectomy,” Cassileth says. “All of these techniques not only produce better results, but provide more choices for patients and allow us to tailor our surgeries to best suit each patient’s needs.”
Richardson created the Goldilocks Mastectomy, a technique for closing a mastectomy on larger breasts. They further advanced that technique to what Cassileth describes as “a nipple-sparing mastectomy reconstruction that only uses one’s natural tissue without an implant and no other surgical sites.”
Their model of care doesn’t end with reconstructive surgeries. The practice is constantly striving to find new and better ways to communicate with patients and ensure that they are addressing prevention and health beyond the physical body. “It’s truly the feeling of concierge medicine where everybody knows your name,” Miller says. “It felt like I had older sisters leading the way with love and compassion.”
Throughout the years, the doctors realized that they could also improve upon routine visits like biopsies and mammograms. Cassileth is ambitious and hopes to expand this cosmetic-forward method of care across the country. “This symbiosis has allowed us to uniquely protect and advocate for best patient outcomes that do not exist elsewhere,” she says. “Our goal is to establish similar dual practices around the country, to allow women to have better outcomes everywhere.”
You Might Also Like

