Everything You Should Know to Keep Breast Cancer out of Your Future

For a disease that has impacted so many people in our lives from mothers, sisters, grandmothers, daughters, friends, and even celebrities like Katie Couric and Olivia Newton-John, there never seems to be enough information out there. We broke down everything you need to know about breast cancer including types of breast cancer, causes of breast cancer, ways to treat breast cancer, how to prevent breast cancer, and more in this all-encompassing guide. So, read on and share, because the more we know, the more we can protect ourselves and those we love.
What is breast cancer?
Breast cancer happens when cells in the breast begin to grow uncontrollably. Just like with other cancers, breast cancer is the result of mutations or abnormal changes in the genes responsible for regulating healthy cell growth. Normally, cells regulate themselves: they grow and divide as your body needs them. When cancer develops, however, this orderly process breaks down—abnormal, old, or damaged cells survive when they should die, and new cells form when they shouldn’t. These extra cells can divide without stopping and may form growths called tumors.
Most breast cancers begin either in the lobules (the breast tissue made up of glands for milk production) or in the ducts that connect the lobules to the nipple. “It usually stays in those areas, but in certain circumstances, it can spread,” says Megan Kruse, M.D., an oncologist at the Cleveland Clinic in Ohio and assistant professor of medicine at the Cleveland Clinic Lerner College of Medicine. “In those cases, the most common places it goes is to the lungs, liver, bone, or brain.”

Breast cancer usually occurs in women, but men can get breast cancer, too. “Because it’s a hormonally driven cancer, most breast cancers need estrogen in order to grow, which is why it’s much more common in women than in men,” says Jennifer Specht, M.D., an oncologist at Seattle Cancer Care Alliance and an associate member of the clinical research division at Fred Hutchinson Cancer Research Center. Only one percent of all the breast cancers diagnosed in the United States is among men, adds Dr. Kruse.
Breast cancer is the most common cancer in American women, except for skin cancers. The average risk of a woman in the United States developing breast cancer in her lifetime is about 13 percent (about a 1 in 8 chance).
The American Cancer Society estimates that in the United States in 2022, approximately 287,850 women will be diagnosed with invasive breast cancer and about 43,250 women will die from it. While breast cancer incidence rates are highest in non-Hispanic white women and Asian/Pacific Islander women, breast cancer death rates are highest in African American women.
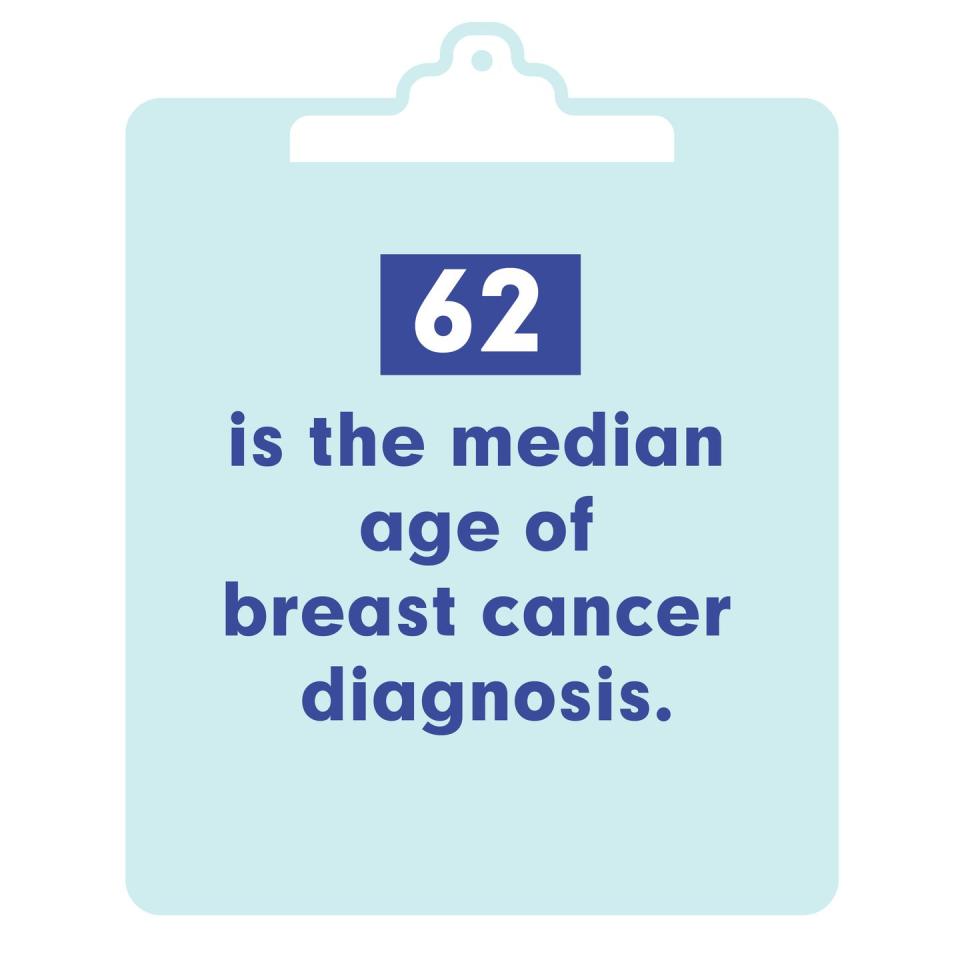
“Most of the breast cancer we see in the United States happens in postmenopausal women, although we are seeing more and more cases now in younger women,” says Dr. Kruse. According to the American Cancer Society, the median age of breast cancer diagnosis is 62, with the median age being slightly younger for black women (60) than for white women (63).
Unfortunately, breast cancer usually has no symptoms when the tumor is small and most easily treated, which is why screening is important for early detection. The most common physical sign is a painless lump. If the cancer has spread to the underarm lymph nodes, it may cause a lump or swelling. “There can also be changes to the breast such as dimpling or puckering of the skin or changes in how the nipple looks,” notes Dr. Specht. “If the nipple becomes retracted, that could potentially be a sign of a problem in the breast.”
What are the types of breast cancer?
There are many types of breast cancer, and they tend to fall into two categories:
In situ: meaning the breast cancers have not spread
Invasive or infiltrating: meaning the cancers have spread into the surrounding breast tissue; 80 percent of breast cancers are invasive or infiltrating
The most common types of breast cancer are:
Ductal carcinoma in situ (DCIS)
When it comes to in situ breast cancers, DCIS makes up about 20 percent of newly diagnosed breast cancers. DCIS happens when abnormal cells replace the normal epithelial cells that line the breast ducts and expand into the ducts and lobules. DCIS may or may not progress to invasive cancer; in fact, sometimes it grows so slowly that it never affects a woman’s health, even without treatment.
Invasive ductal carcinoma (IDC)
Invasive breast cancers are the most common type of breast cancer overall, making up 70 to 80 percent of cases. Of those, IDC is the most common, comprising 8 out of 10 cases. IDC starts in the cells that line a milk duct in the breast. It breaks through the wall of the duct and grows into nearby breast tissues. From there, it can spread (metastasize) to other parts of the body through the lymph system and bloodstream.
Invasive lobular carcinoma (ILC)
This type of breast cancer in the second most common type starts in the lobules (milk-producing glands) and accounts for approximately 5 to 10 percent of all breast cancers. ILC may be harder to detect than IDC via a physical exam or imaging, like mammograms. And compared to other kinds of invasive carcinoma, about 1 in 5 women with ILC might have cancer in both breasts. Like IDC, it can spread to other parts of the body.
Other types of breast cancer
There are other, less common, types of breast cancers, too, such as sarcomas, phyllodes, Paget disease, and angiosarcomas which start in the cells of the muscle, fat, or connective tissue. For more information on the various types of breast cancer, check out this guide to types of breast cancer.
What causes breast cancer?
Experts still aren’t fully sure what triggers the gene mutations that cause breast cancer—but they do know there are several breast cancer risk factors that up your odds of contracting this disease. “When we think about breast cancer, we try to break it down into things you can and can’t change,” says Dr. Kruse. “There are risk factors you’re born with and then there are others that you can actually do something about.” In many cases, those lifestyle-related risk factors are not all that difficult to change.
Remember: Not all women who have a risk factor—or even multiple risk factors—will develop breast cancer. And some women who have no known risk factors still end up being diagnosed.
Lifestyle-related breast cancer risk factors you can control
Being overweight or obese
Not exercising
Having kids later in life
Not breastfeeding
Taking birth control
Using hormone therapy after menopause
Breast cancer risk factors you cannot change
Being assigned female at birth
Getting older
Having certain inherited genes
Having a family history of breast cancer
Having breast cancer in the past
Your race and ethnicity
Having dense breast tissue
Getting your period early
Going through menopause after 55
Having radiation to your chest as a kid
Exposure to DES (a synthetic form of estrogen)
What are the symptoms of breast cancer?
The most common sign of breast cancer is a painless, hard lump or mass with irregular edges. It’s important do a self breast exam regularly, but there are breast cancer symptoms that have nothing to do with a lump. Here are additional symptoms to look out for:
Sometimes breast cancer can spread to the lymph nodes under the arm or around the collar bone and cause a lump or swelling there. “If you notice any fullness or lumps under the arm that don’t come and go, that’s a concerning sign and you should get checked by a healthcare provider,” says Dr. Kruse. In general, she notes that a lot of the symptoms of breast cancer, even lumps or pain, are hard to distinguish on your own so if you notice any change in your breasts, see your doctor.
How is breast cancer diagnosed?
If you go to your doctor with a breast concern or complaint, the first thing they’ll likely do is a physical exam to see how the breast in question compares to your other breast, says Dr. Kruse. “They’ll also ask questions about your menstrual status and caffeine intake, as these are things that can make you have normal lumps in the breast that come and go,” she adds.
If, after that, your doctor is concerned, they will recommend a mammogram and ultrasound to get a better look at the lump or change in the breast. If these tests show an abnormality, you’ll likely need a biopsy—a procedure where the breast tissue in question is removed so the cells can be looked at in a lab to see if they’re cancerous. The American Cancer Society notes that needing a breast biopsy doesn’t necessarily mean you have cancer, and most biopsy results are not cancer.
There are different kinds of breast biopsies but the most common is a needle biopsy—an outpatient procedure where a radiologist uses a small needle to get a sample of the abnormal breast tissue. “This allows a pathologist to look at the cells under the microscope and make the diagnosis of breast cancer,” explains Dr. Specht. It usually takes a few days to get the results.
Stages of breast cancer
If you’re diagnosed with breast cancer, your doctor will immediately try to figure out if it has spread, and if so, how far, according to the American Cancer Society. This process is called “staging,” and it helps determine how serious the cancer is and how to treat it. “We stage it based on the size of the tumor in the breast and whether or not the cancer has spread to the lymph nodes or another organ in the body,” says Dr. Specht. “The stage of breast cancer dictates how we treat it even more than which type it is.”
The earliest stage of breast cancer is stage 0 (carcinoma in situ); from there, it ranges from stage I through IV. As a rule, the lower the number, the less the cancer has spread.
Here is more information about each stage:
Stage 0
Also called pre-cancer, this is the earliest stage of breast cancer. It usually begins in the breast ducts or milk glands and has stayed there, which means it’s not invasive (it hasn’t spread to other breast tissue or to the lymph nodes). However, it could become invasive cancer in the future.
Stage I
Starting at this level, breast cancer is called invasive, meaning it has started spreading to healthy breast tissue. Stage IA means the tumor measures up to 2 centimeters but has not spread outside the breast, and no lymph nodes are involved. Stage IB means either there’s no tumor or the tumor is less than 2 centimeters, and small clusters of breast cancer cells are found in the lymph nodes.
Stage II
At stage II, the cancer has grown, spread, or both. This stage has two subcategories: IIA and IIB.
Stage IIA
No tumor but cancer larger than 2 millimeters is present in the lymph nodes under the arm or near the breastbone, or
A small tumor (no more than 2 centimeters, or roughly 3/4 of an inch) and cancer in the lymph nodes, or
A tumor of 2 to 5 centimeters but no lymph node involvement
Stage IIB
A tumor of 2 to 5 centimeters and small clusters of breast cancer cells in the lymph nodes
A tumor between 2 and 5 centimeters and cancer that has spread to up to four lymph nodes
A tumor larger than 5 centimeters and no lymph node involvement
Stage III
At this stage, the cancer is more advanced and has spread to the lymph nodes but not other organs. Stage III has three subcategories: IIIA, IIIB, and IIIC. Each category is based on tumor size and lymph node involvement.
Stage IIIA
There is no tumor in the breast or the tumor may be any size; cancer is found in 4 to 9 axillary lymph nodes or in the lymph nodes near the breastbone, or
the tumor is larger than 5 centimeters and small groups of breast cancer cells (no larger than 2 millimeters) are found in the lymph nodes, or
the tumor is larger than 5 centimeters and cancer has spread to 1 to 3 axillary lymph nodes or to the lymph nodes near the breastbone
Stage IIIB
the tumor may be any size and has spread to the chest wall and/or skin of the breast and caused swelling or an ulcer, and
It may have spread to up to 9 axillary lymph nodes or may have spread to lymph nodes near the breastbone
Stage IIIC
there may be no sign of cancer in the breast or, if there is a tumor, it may be any size and may have spread to the chest wall and/or the skin of the breast
The cancer has spread to: 10 or more axillary lymph nodes, lymph nodes above or below the collarbone, or axillary lymph nodes or to lymph nodes near the breastbone
Stage IV
Also known as metastatic breast cancer, at stage IV, the cancer has spread (or metastasized) to other organs, most often the bones, lungs, liver, and brain.
How is breast cancer treated?
There are many different breast cancer treatments, based on the type and stage, and many women get more than one type of treatment. There are “local treatments,” meaning they treat the tumor without affecting the rest of the body, and “systemic treatments,” which can reach cancer cells throughout the body. Here’s a breakdown of each treatment:
Local breast cancer treatments
Surgery
Most women will need surgery as part of their breast cancer treatment, says Dr. Kruse. “It can be anything from just removing the cancer itself to removing the whole breast,” she explains. You might opt for a lumpectomy, for example, where only the part of the breast containing the cancer is removed or a mastectomy, which is the removal of the entire breast.
Radiation
Radiation therapy is treatment with high-energy rays (such as x-rays) or particles that destroy cancer cells. The two main types to treat breast cancer are: external beam radiation (which comes from a machine) and internal radiation (where a radioactive source is put inside the body for a short time). Not all women will need radiation but it is most often used after surgery to reduce the risk that the cancer will return.
Strangers with metastatic breast cancer describe their very different treatment choices:
Systemic breast cancer treatments
Chemotherapy
Administered intravenously (through your vein) or by mouth, chemo is treatment with cancer-killing drugs that travel through the bloodstream to reach cancer cells all over the body. Not all women with breast cancer will need chemo but it is most commonly used: after surgery (to kill any cancer cells that may have been left behind), before surgery (to try to shrink the tumor so it may be more readily removed), or for advanced (metastatic) breast cancer.
Hormone therapy
This treatment is recommended for women with hormone receptor-positive (ER-positive and/or PR-positive) breast cancers and it involves taking drugs (such as tamoxifen) that stop estrogen from stimulating breast cancer cell growth. Hormone therapy is often used after surgery to help reduce the risk of the cancer coming back but it is sometimes used before surgery, as well. It’s usually taken for at least five years.
Targeted therapy
These are targeted drugs designed to block the growth and spread of cancer cells. They work differently than chemotherapy drugs and can sometimes work when chemo does not (they also have different side effects). Targeted therapy is most often used if you have HER-2 positive breast cancer, hormone receptor-positive (ER-positive or PR-positive) breast cancer, or if you have BRCA gene mutations.
How to prevent breast cancer
Unfortunately, there’s no silver bullet when it comes to preventing breast cancer. And though there have been some trial vaccines, in the meantime, there are steps you can take to lower your risk. Here are some good guidelines to follow:
Maintain a healthy diet
Both increased body weight and weight gain as an adult are linked with a higher risk of breast cancer after menopause, according to the American Cancer Society. Following a healthy diet full of fruits, vegetables, whole grains, and lean protein can help give your body the fuel it needs to maintain a healthy weight and the nutrients it needs to stay cancer-free. Recent research suggests foods that are highly inflammatory can increase the risk of breast cancer. Talk to your doctor and work with a dietitian to follow a diet that allows you to maintain a healthy body weight for you.
Exercise regularly
Many studies have shown that moderate to vigorous physical activity is linked with lower breast cancer risk. The American Cancer Society recommends that adults get at least 150 minutes of moderate-intensity to vigorous-intensity activity each week, preferably spread throughout the week.
Limit your alcohol intake
Even low levels of alcohol intake have been linked with an increased risk of breast cancer. The American Cancer Society recommends that women have no more than one alcoholic drink a day (they define a drink as 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of hard liquor).
Breastfeed if you can
Women who choose to breastfeed for at least several months may also get the added benefit of reducing their breast cancer risk.
If you have a very high risk for breast cancer (due to a strong family history of breast cancer, a known gene mutation such as the BRCA 1 or BRCA2 gene, or you have DCIS or LCIS), you may want to consider prescription medications that can lower breast cancer risk or preventative surgery (such as a prophylactic mastectomy) or a procedure to remove the ovaries, which are the main source of estrogen in the body. While surgery can lower the risk of breast cancer, it can’t eliminate it completely, and it can come with a host of side effects so talk to your doctor to find out what’s right for you.
You Might Also Like

