Foods to Eat And Avoid With Diverticulitis
Dietary Recommendations for Better Management
Medically reviewed by Jay N. Yepuri, MD
Diverticulitis is a condition in which the diverticula, small, bulging pouches or sacs that grow inside the walls of your colon (large intestine), get inflamed or infected. It's not known exactly what causes diverticulitis flare-ups, but risk factors include:
Having had an episode of diverticulitis in the past
Eating red meat regularly
Having a low-fiber diet
Smoking
Being overweight
Lack of physical activity
Aging
Taking certain medicines, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and steroids
The diverticulitis diet includes foods to eat during a flare-up and recovery. With a flare-up, experts recommend a clear liquid diet for a few days. During recovery, you will slowly reintroduce low-fiber solid food, like white bread and low-fiber cereal, back into your diet.
Once you are feeling better, the standard recommendation is to eat foods high in fiber with little or no red meat. However, you should add fiber to your diet slowly. You may want to keep a food journal to record what you eat and how you feel.
This article provides an overview of the diverticulitis diet. It explains what you should eat during a diverticulitis flare-up and foods to avoid if you have the condition. It also details how to slowly add fiber to your diet to avoid a painful recurrence of symptoms.
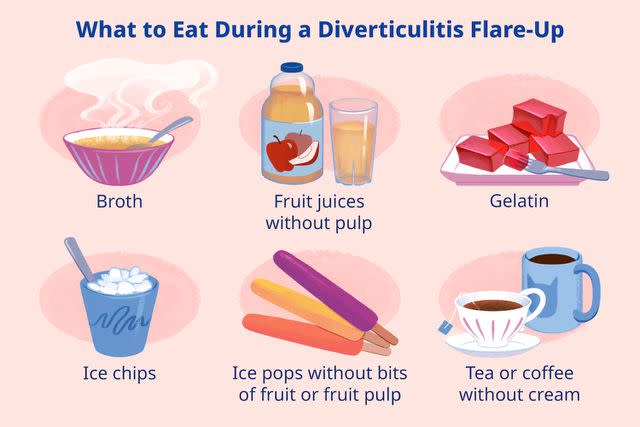
Illustration by Mira Norian for Verywell Health
Foods to Eat During a Diverticulitis Flare-Up
During a diverticulitis flare, you may need to give your bowel time to rest. This typically means ingesting only clear liquids for a few days.
Liquid Diet
Foods to include in the initial phase of a diverticulitis flare-up include:
Broth
Fruit juices without pulp, such as apple juice
Gelatin
Ice chips
Ice pops without bits of fruit or fruit pulp
Tea or coffee without cream
Water
A liquid diet should only be followed for a few days before transitioning to the next phase.
Related: 10 Diverticulitis Self-Care Tips and Home Remedies
Foods to Eat During Recovery From Diverticulitis
A low-fiber or low-residue diet is recommended during recovery from a diverticulitis attack.
Low-Fiber and Low-Residue Foods
Also known as a soft diet, foods included in this temporary healing diet include:
Starchy foods: White bread, white rice, potatoes (no skin)
Dairy: Milk, cottage cheese
Protein: Eggs, fish, lean poultry, yogurt, gelatin
Fruit: Applesauce, canned or cooked fruit, fruit juice (no pulp)
Vegetables: Well-cooked vegetables
Liquids: Broth, ice pops
Foods to Avoid With Diverticulitis
While you're recovering from a flare-up, avoid foods that are high in fiber. These include:
Beans and legumes: Lentils, split peas, pinto beans, black beans, etc.
Whole grains: Whole wheat, oats, quinoa, brown rice, farro, wheat berries, etc.
Whole-grain products: High-fiber cereals, bran, shredded wheat, granola, whole-grain breads, whole-wheat pasta
Nuts and seeds: Almonds, walnuts, pumpkin seeds, chia seeds, etc.
Fruit: Raw or dried fruit or juice with pulp
Vegetables: Uncooked vegetables, potato skins
Processed meats: deli meats, salami, hot dogs, sausage, bacon
Crunchy peanut butter
Fried or spicy foods
When Can I Return to a Normal Diet?
Once your diverticulitis symptoms resolve, you can gradually add foods back into your diet. However, it may take a week or longer until you return to your regular way of eating. Your healthcare provider will let you know when and how to resume eating a normal diet.
High-Fiber Diet to Prevent Diverticulitis
After you have recovered from a diverticulitis attack, your healthcare provider will recommend adding more fiber to your diet. Eating more fiber or taking fiber supplements can help prevent future attacks.
This is because fiber softens stool and helps prevent constipation. Avoiding constipation aids in decreasing pressure in the colon, which may prevent future diverticulitis flare-ups.
However, when you first set out to eat more fiber, go slowly. Start by eating 5 to 15 grams of fiber a day. Add a little fiber to your diet at a time and gradually work up to a higher daily intake. If you have bloating or gas, reduce the amount of fiber you eat for a few days.
As you add more fiber, be mindful of your fluid intake. Fiber requires water to work properly. If you don't drink enough water, stools can become too firm and hard to pass.
How Much Fiber Do I Need?
The average adult eating a 2,000-calorie diet needs at least 28 grams of fiber each day.
High-fiber foods recommended to prevent diverticulitis include:
Beans and legumes
Bran, whole wheat bread, and whole grain cereals such as oatmeal
Brown rice, quinoa, and barley
Fruits such as berries, apples, pears, kiwis, and oranges
Vegetables such as broccoli, cauliflower, carrots, and dark leafy greens (kale, collard greens, Swiss chard, and spinach)
Whole wheat pasta
Popcorn
Nuts and seeds
Meal Timing
Some people with digestive disorders feel better eating smaller portions more frequently rather than sitting down to three larger meals a day.
However, this is highly individualized, and there is no standard recommendation for meal timing with diverticular disease. It may take some experimenting with different meal timing and quantities of food to find what works best.
Related: How Your Digestive System Works
How Certain Foods Affect Diverticulitis
Since each person's diverticulitis is individualized, there is no scripted plan that is sure to help you. There are basics that can guide recommendations, but some of this may prove to be trial and error.
Beverages
Proper hydration helps prevent constipation and helps process the extra fiber you’re eating. Drink at least 8 to 10 cups of water per day to help prevent constipation. Also, pay attention to whether or not other drinks cause or worsen your symptoms.
Beverages that bother some people with diverticular disease include:
Coffee
Tea
Soda
Wine and other alcoholic drinks
Some people only need to avoid certain drinks when recovering from a flare, while others find they need to always avoid them to keep symptoms at bay.
Nuts, Seeds, and Popcorn
In the past, people with diverticulosis were advised to avoid these foods because it was thought they would get caught in the diverticula and lead to diverticulitis.
However, research now indicates these foods don’t specifically cause inflammation of the pouches. That's good news, as they are very good sources of fiber.
Fruit
Fresh fruits, like apples and pears, have the most fiber when eaten with the skin. However, if you’re having symptoms of diverticulitis, look for lower-fiber options, like applesauce.
Bananas are another good source of fruit fiber. They also have a lot of potassium and can be especially helpful if you’re recovering from a stomach upset.
If you're prone to constipation, avoid unripe bananas. Research shows bananas that are still a bit green, unblemished, and firm are more likely to be binding (which makes stools firmer) due to higher levels of tannins and resistant starch. Instead, reach for bananas that are softer and spotted, which are easier to digest.
Dairy
If you tolerate dairy, add non-fat or low-fat milk, yogurt, and cheese to your diet. (Even if you aren’t lactose intolerant, full-fat dairy may be harder to digest.)
When you're experiencing a flare-up, especially if you have diarrhea, you may prefer to avoid dairy until you’re feeling better. Lower-lactose dairy products, like cottage cheese and yogurt, may be tolerable.
Grains
Whole grains are one of the best sources of dietary fiber. Choosing whole-grain bread, crackers, pasta, and brown rice can be a nutritious, tasty, and versatile way to add fiber to your diet.
However, when you aren't feeling well, stick to low-fiber foods such as refined white bread, white rice, and crackers until your symptoms improve.
Protein
Lean ground poultry and eggs are great protein sources whether you're having symptoms or you're feeling well. You can also experiment with higher-fat sources of protein, like nuts and nut butter. However, they might not be the best choice during a symptom flare.
Vegetables
When you're symptom-free and eating a high-fiber diet, raw vegetables (especially root and cruciferous veggies) are nutritional powerhouses.
However, when symptomatic, you may want to avoid them. For example, if you're experiencing a flare, a baked sweet potato with the skin may be too hard to digest. Instead, a peeled, mashed white potato may be easier on your system.
Red Meat
After you've recovered from a diverticulitis attack, you may want to avoid red meat, including beef, pork, lamb, and venison. Red meat is linked to an increased risk for diverticulitis, though the exact reason is unclear.
Studies show red meat alters the balance of microorganisms in the cecum—a pouch in the digestive tract where the small and large intestines meet. Researchers suspect this may trigger inflammation associated with diverticulitis.
Spices
Ginger, turmeric, and garlic have anti-inflammatory properties, and ginger is a popular remedy for soothing stomach upsets.
However, some spices can be irritating to the lining of the gastrointestinal tract. You may want to avoid them after an acute episode of diverticulitis. Then start with small amounts and increase according to your comfort level.
Related: Is There Something Wrong With Your Bowels?
Diverticulitis Diet vs. Other Diets
Two major factors that impact diverticulitis are inflammation and maintaining healthy bowel movements. Diet impacts both of these and changing what you eat can help manage diverticulitis or reduce the risk of developing diverticula in the first place.
The diverticulitis diet is often recommended because it reduces inflammation by eliminating or limiting certain inflammatory foods and promotes regular bowel movements. which may prevent diverticulitis in the future.
The diet for diverticulitis is similar to several diets prescribed for bowel rest after surgery. These diets can also be used by people who have chronic inflammatory bowel disease, have an acute gastrointestinal illness, or are recovering from a medical emergency such as a bowel obstruction.
The BRAT Diet
The BRAT diet generally consists of bananas, plain white rice, applesauce, and toast made with refined white bread. When your digestive system needs rest, eating a diet of soft but nutritious food can mitigate symptoms like nausea and diarrhea while giving your body time to heal.
Low-FODMAP Diet
A low-FODMAP Diet is low in the fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) present in varying amounts in the food you eat. Foods high in FODMAPs cause some people to experience cramps, gas, bloating, diarrhea, or constipation. Paying attention to whether high-FODMAP foods affect your diverticulitis symptoms may be helpful in the long term.
Learn More: The Low-FODMAP Diet
Summary
Modifying your diet is an excellent first step to taking control of diverticulosis and diverticulitis. Dietary changes can help manage your symptoms and reduce diverticulitis flares.
Everyone’s body is different, and the diet that works for you may not work for someone else with diverticulitis. Over time, you can learn how to modify your diet or make other changes to your lifestyle to ensure you can manage your condition and overall health and well-being.
Read Next: Managing IBS and Diverticulosis at the Same Time
Read the original article on Verywell Health.

