What Is Dysphagia?
A Swallowing Impairment With Several Potential Causes
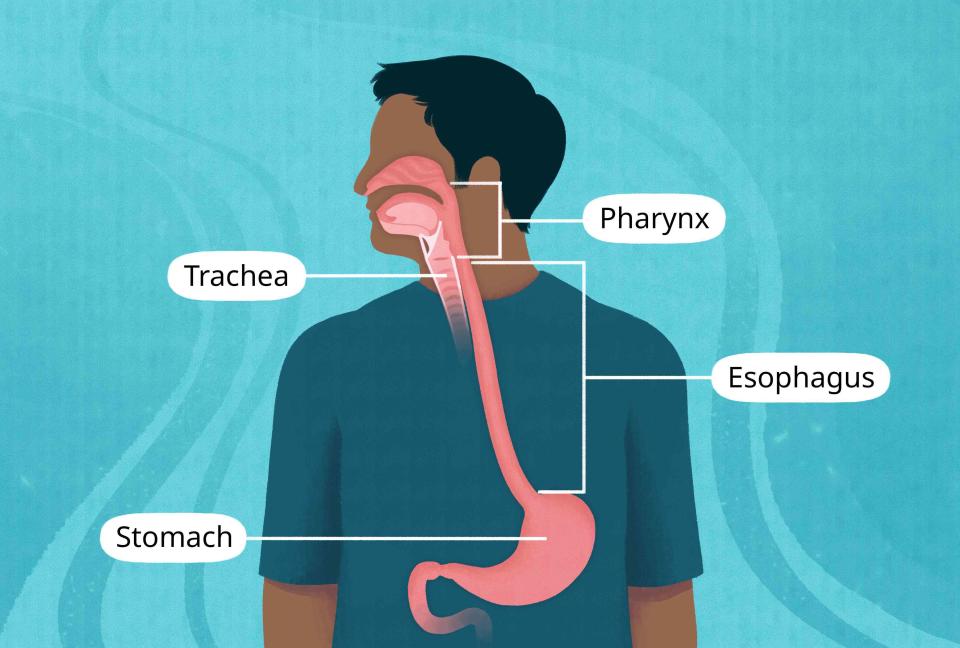
Illustration by Mira Norian for Verywell Health
Medically reviewed by Reza Samad, MD
"Dysphagia" means "difficulty swallowing." It has many possible causes, including an underlying nerve or muscle disorder or obstructive issues like an abnormal growth within the throat or esophagus (food pipe).
Pinpointing the cause of and managing dysphagia is paramount to ensuring your health and preventing complications like malnutrition, dehydration, and social isolation.
This article will discuss what dysphagia feels like, how it's diagnosed, and its treatment options.
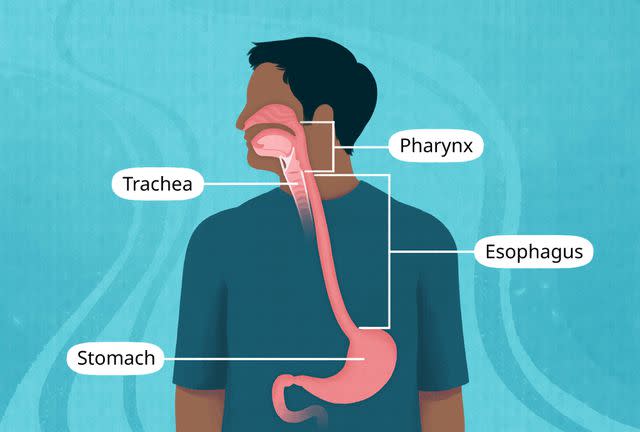
Illustration by Mira Norian for Verywell Health
Dysphagia: When You Have Trouble Swallowing Food
Possible symptoms of dysphagia include:
Difficulty initiating or completing a swallow
Coughing, choking, gagging, or drooling when eating or drinking
Feeling like food is stuck in the throat or chest after eating
Nasal regurgitation (bringing up swallowed food/fluids through the nose)
Pain when swallowing (odynophagia)
Heartburn (burning sensation behind your breastbone) or chest pain
Hoarseness or a change in breathing pattern or voice quality
Related:What's Causing Me to Cough After I Eat?
Dysphagia Causes: Why Is It Hard to Swallow?
There are two main types of dysphagia, and within these types are several possible causes.
Oropharyngeal Dysphagia
Oropharyngeal dysphagia stems from a swallowing problem within the oropharynx, the medical term for the mouth and the structures located at the back of the throat (e.g., tonsils and end of your tongue).
Long-term neurological conditions like Parkinson's disease, stroke, and Alzheimer's are common causes of oropharyngeal dysphagia.
Neuromuscular disorders (related to muscle/nerve problems in the body), like multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS), and myasthenia gravis (MG), can also cause oropharyngeal dysphagia.
Structural problems that press on or otherwise interfere with the tissues/muscles involved in swallowing are additional causes. Example include:
Bone spurs in the neck (cervical osteophytes)
Zenker's diverticulum (the muscle between the throat and esophagus becomes overly tight, causing a pouch at the back of the throat)
Goiter (abnormal enlargement of the thyroid gland)
Medications may also cause or contribute to oropharyngeal dysphagia, such as antipsychotic drugs, antihistamines, or diuretics.
Esophageal Dysphagia
Esophageal dysphagia stems from a swallowing problem within the esophagus, the hollow tube that carries food from the mouth to the stomach.
Two common causes of esophageal dysphagia include:
Gastroesophageal reflux disease (GERD) is when stomach acid backs into the esophagus. Common symptoms include heartburn and regurgitation.
Eosinophilic esophagitis is a chronic inflammatory condition associated with a buildup of eosinophils (type of white blood cell) in the esophagus. It's believed to stem from food allergies or environmental allergies.
Structural problems or anything that physically blocks the esophagus can also cause dysphagia. Examples include:
A foreign body or impacted food
Esophageal narrowing (stricture)
A ring of tissue that forms near the end of the esophagus (Schatzki ring)
Pill-induced esophagitis is another reason for esophageal dysphagia. It results from injury to the tissue lining the esophagus caused by taking certain medications.
Drugs linked to pill-induced esophagitis include:
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as Advil or Motrin (ibuprofen)
Tetracyclines (an antibiotic, for example, doxycycline)
Bisphosphonates (used to treat osteoporosis, a disease of bone thinning)
Ascorbic acid (vitamin C)
Functional esophageal disorders like Globus sensation (feeling a painless lump in the throat) may also cause problems swallowing. The cause behind functional esophageal disorders remains unknown, although experts suspect overly sensitive nerve cells communicating sensory information to the brain may be involved.
Lastly, while rare, an esophagus infection or esophageal motility disorder like achalasia (when the nerves in the esophagus malfunction) can cause dysphagia.
Understanding the Stages of Swallowing
The swallowing process is highly complex and involves the brain and muscles within the mouth, throat, voice box, and esophagus.
Swallowing can be divided into two primary stages—the oropharyngeal and esophageal stages. When evaluating dysphagia, sorting out which stage the swallowing impairment occurs is a key first step.
This step involves carefully assessing the following:
Symptoms, including their timing (e.g., intermittent or slowly/rapidly getting worse)
Whether the swallowing impairment occurs with solids, liquids, or both
Presence of alarm symptoms (e.g., weight loss)
Past medical history (e.g., food allergies or acid reflux)
Vitamins, supplements, and medications the person is taking
Once the stage of swallowing impairment is determined, various diagnostic tests may be performed to help reach a precise diagnosis.
Two examples of tests used to assess dysphagia include:
A modified barium swallow uses X-rays to analyze the way you swallow different food consistencies (e.g., liquids, thickened liquids, and solids)
Fiberoptic endoscopic evaluation of swallowing (FEES) is a procedure in which a person's swallowing ability is examined using a flexible tube with a tiny camera attached to the end that's placed through the nose.
Oropharyngeal Stage
In this stage, food is first chewed and mixed with saliva in the mouth to form a bolus (mass of food).
The tongue then propels the bolus or fluid into the throat, followed by a rapid transfer of the solid or liquid material into the upper part of the esophagus.
As the foods/fluids navigate the esophagus, the nasopharynx (the upper part of the throat connected to the nose) and the larynx (voice box) are sealed off. This seal prevents food or fluids from backtracking into the nose, airways, or lungs.
Also going on during this time is the relaxation of the lower esophageal sphincter (a one-way valve). This relaxation is in preparation for the passage of food or fluid into the stomach.
Symptoms supporting a problem in the oropharyngeal stage include:
Choking, coughing, drooling, and nasal regurgitation
Hoarseness or other voice changes
Difficulty swallowing liquids only
A hard time chewing foods (e.g., severe dry mouth or neuromuscular disease)
Esophageal Stage
In this stage, muscles propel the food bolus and fluids through the rest of the esophagus, emptying it into the stomach through the relaxed lower esophageal sphincter.
The highly coordinated series of muscle movements that pushes foods or fluids through the esophagus is called peristalsis.
Peristalsis is controlled by a region in your brainstem called the medulla oblongata. It's an involuntary movement, meaning it's done reflexively, out of your conscious control.
Symptoms supporting a problem in the esophageal stage include:
Feeling like food is stuck in the throat or chest
Difficulty with swallowing solids only (e.g., esophageal stricture)
Difficulty swallowing both solids and liquids (e.g., achalasia)
Treatment to Get Dysphagia to Go Away
Treating dysphagia is essential as it can lead to serious complications, including weight loss, dehydration, and aspiration pneumonia (when food enters the lungs leading to an infection). In older adults, dysphagia is also linked to a reduced life expectancy and decreased quality of life.
The treatment of dysphagia depends on the underlying diagnosis. It may include lifestyle changes, medication, swallowing rehabilitation, or surgery.
While not an exhaustive list, examples of dysphagia therapies include the following.
Lifestyle Behaviors
For GERD, lifestyle interventions like weight loss (if overweight or have obesity) and avoiding smoking are usually advised.
For eosinophilic esophagitis, eliminating major food allergens from the diet (e.g., dairy, egg, wheat, soy, peanut/tree nuts, and fish/shellfish) may be recommended.
Treatment of pill-induced esophagitis involves stopping the offending drug. If this is not possible, instructions on properly taking the pill are emphasized (e.g., sitting upright for at least 30 minutes after swallowing).
Related:How to Dislodge a Pill Stuck in Your Throat
Medications
A healthcare provider may recommend the following medications for dysphagia:
A proton pump inhibitor, such as Prilosec (omeprazole) for GERD or eosinophilic esophagitis
Dupixent (dupilumab) injection and/or swallowing small doses of steroids (e.g., budesonide) to counter the inflammation for eosinophilic esophagitis
An antiviral, antibiotic, or antifungal drug for an esophagus infection
Swallowing Rehabilitation
You may be asked to see a swallowing therapist, sometimes called a speech-language pathologist, especially if you have oropharyngeal dysphagia from a neurological condition.
A swallowing therapist can teach you exercises to strengthen your jaw, lip, and tongue. They can also teach techniques to help you swallow more efficiently and safely.
Learn More:Swallowing Exercises for Dysphagia From Neurological Causes
Your therapist will also teach you how to chew thoroughly, take smaller bites, and coat foods with fluids or sauces to assist in swallowing. They will also review specific foods on a mechanical soft diet or pureed diet.
Examples of foods on a mechanical soft diet include:
Milk, milkshakes, and cottage cheese
Mashed potatoes, diced soft pasta, and cooked cereal
Fruit and vegetable juices
Creamed spinach and applesauce
Hummus or soft chicken salad
Ice cream and frozen yogurt
Liquid nutritional supplements like Ensure
Surgical Procedures/Surgery
An operation may be required to remove harmful tissue (e.g., cancer) or other structural abnormality in the throat, esophagus, or surrounding area.
Various surgical procedures may also be recommended to manage dysphagia. For example, with esophageal strictures, gentle widening of the esophagus using a balloon dilator during endoscopy may be performed.
Learn More:How Esophageal Dilation Helps Difficulty Swallowing
Managing Chronic Dysphagia
Dysphagia can be acute or chronic, depending on the fundamental cause.
Neurological or neuromuscular conditions, like stroke, Parkinson's disease, and ALS, are examples of chronic causes of dysphagia. Unlike acute causes, which in many cases can be reversed (e.g., pill-induced esophagitis), chronic causes of dysphagia can either improve or worsen.
For example, dysphagia from stroke usually improves with time and swallowing rehabilitation, whereas dysphagia from Parkinson's disease or ALS slowly progresses over time due to the disease's natural course.
Managing chronic, progressive dysphagia requires a team, including healthcare providers like a swallowing therapist and primary care physician, as well as the person and their family members or caregivers.
A palliative care specialist (a doctor who aims to relieve symptoms of serious illnesses) is also often involved, especially as the disease advances.
The goals of managing chronic dysphagia involve preventing complications and optimizing the patient's comfort and quality of life.
Related:Diet and Nutrition for ALS
Summary
"Dysphagia" means "difficulty swallowing," and symptoms may include a sensation of food being stuck in the throat or chest or choking and coughing when eating or drinking.
There are numerous causes of dysphagia depending on where the swallowing impairment is located (e.g., mouth, throat, or food pipe) and whether other factors are present, notably an underlying condition (e.g., acid reflux or stroke).
Managing dysphagia may entail lifestyle modifications, swallow rehabilitation, medication, and/or surgery. Depending on the dysphagia diagnosis, swallowing techniques and adopting a soft or pureed diet may also be helpful.

