Diverticulitis Flare-Ups
Symptoms and how to get relief

Illustration by Tara Anand for Verywell Health
Medically reviewed by Jay N. Yepuri, MD, MS
A diverticulitis flare-up occurs when the pouches in your colon wall (diverticula) become inflamed or infected.
This can cause symptoms such as abdominal pain (often on the lower left side), fever, cramping, diarrhea, or constipation. In severe cases, rectal bleeding may occur.
This article discusses what might cause a diverticulitis flare-up (sometimes called a diverticulitis attack), how to know you are having one, and how a flare-up is diagnosed and treated.
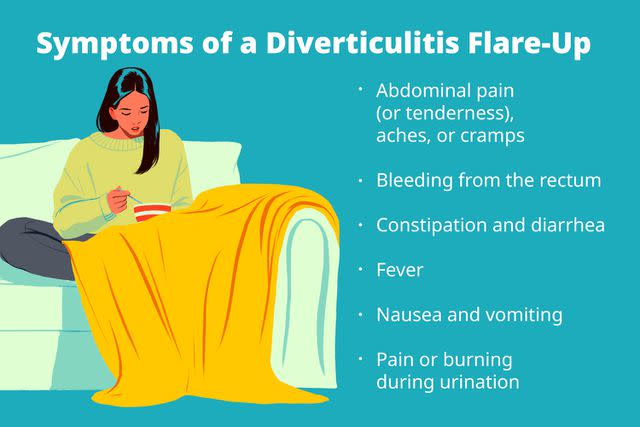
Illustration by Tara Anand for Verywell Health
Symptoms of a Diverticulitis Flare-Up
Some of the signs and symptoms of a diverticulitis flare-up include:
Abdominal pain, aches, or cramps, typically on the lower-left side
Abdominal tenderness
Bleeding from the rectum
Fever
Nausea
Pain or burning during urination (sometimes)
Vomiting
Flare-up symptoms typically resolve within a few days once treatment is started. Approximately 20% of people who experience one flare-up will have another one.
What Causes Diverticulitis Flare-Ups?
It's not known exactly what causes or triggers a diverticulitis flare-up, but risk factors may include:
Having had an episode of diverticulitis in the past
Eating red meat regularly
Not including enough fiber in the diet
Smoking
Being overweight
Aging
It’s currently thought that the risk of an acute flare-up of diverticulitis is under 5%. In the United States, around 200,000 people are hospitalized for diverticulitis each year.
How Diverticulitis Is Diagnosed
If you already know you have diverticulosis, diverticulitis might be suspected right away if you have symptoms of a flare-up. Still, it’s important to know what is causing the symptoms so they can be treated and complications prevented.
The first step in the diagnosis of a diverticulitis flare-up involves your healthcare provider asking questions about your medical history and symptoms. For example, you will be asked questions such as:
How bad is the pain?
Where is the pain located?
Are you experiencing any bleeding?
Are you experiencing constipation or diarrhea?
Based on a review of your symptoms, your provider may recommend some of the following tests:
Blood tests: A blood test might show if there are more white blood cells than there should be, which could mean an infection.
Computed tomography (CT) scan: This is a type of X-ray that’s used to see the organs in the abdomen in cross-section, including the large intestine.
Magnetic resonance imaging (MRI): An MRI uses a strong magnet to create images of the abdominal organs.
Stool tests: Diverticulitis won’t be diagnosed with just a stool test, but stool will be tested for infection or other conditions that can cause symptoms.
Ultrasound: An ultrasound is a type of test that uses sound waves to make an image of the organs inside the abdomen.
Ruling Out Other Possibilities
Some of the symptoms of a diverticulitis flare-up can overlap with other diseases. Therefore, it is important to rule out other possible causes.
Some of the conditions that might also be considered when diagnosing diverticulitis are:
Abdominal aorta rupture or dissection: A rare condition where there is a tear in the wall of the aorta, the largest artery in the body
Appendicitis: An inflammation of the appendix
Cholecystitis or cholelithiasis: An inflammation of the gallbladder or the presence of gallstones
Colon cancer: A tumor or growth that begins in the colon
Ectopic pregnancy: A fertilized egg that attaches outside the uterus, resulting in a pregnancy that cannot result in a live birth and that endangers the pregnant person
Incarcerated hernia: A portion of the small intestine that pushes into the groin
Inflammatory bowel disease (IBD): A group of diseases, including Crohn’s disease and ulcerative colitis, that cause inflammation primarily in the digestive system
Irritable bowel syndrome (IBS): A condition that causes diarrhea or constipation and pain in the large intestine
Mittelschmerz: Pain in the abdomen that occurs when an egg is released from the ovary
Ovarian cyst: A fluid-filled sac in or on an ovary
Pancreatitis: Inflammation of the pancreas
Pelvic inflammatory disease: An infection of the uterus, fallopian tubes, or ovaries
Salpingitis: An infection of the fallopian tubes
What to Do When Diverticulitis Flares Up
A diverticulitis flare-up can often be treated at home.
For very mild symptoms of pain, diarrhea, or nausea, a clear liquid diet is often the first step. This should only be done on the advice of a healthcare provider because a liquid diet doesn’t provide enough calories or nutrients for most people on a long-term basis.
If symptoms improve, more foods will slowly be added back into the diet.
Abdominal pain can be treated with Tylenol (acetaminophen). It is thought that aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs), such as Advil (ibuprofen) and Aleve (naproxen), may increase the risk of a future flare-up.
A heating pad may also be used to soothe abdominal pain.
For more serious symptoms, a healthcare professional may prescribe antibiotics to clear up or prevent any infection.
Related:Foods to Avoid With Diverticulitis
Medical Intervention
If the diverticulitis flare-up can’t be managed at home, hospitalization might be needed. You may need intravenous fluids and antibiotics, as well as pain medication or other treatments.
In rare cases, surgery may be necessary if serious complications develop. This could mean removing the part of the bowel with the inflamed diverticula. It could also mean creating an ostomy so stool is diverted away from the affected part of the bowel.
Prevention
It may or may not be possible to prevent diverticulitis, but these lifestyle measures may help:
Getting regular exercise
While it was once thought that nuts, popcorn, or seeds could increase the risk of a diverticulitis flare-up, that has been disproven.
Summary
Diverticular disease is common and doesn’t usually cause any symptoms. When diverticula become inflamed, however, they can cause symptoms such as abdominal pain, fever, or diarrhea. This is called a diverticulitis flare-up.
Diet changes may be enough to manage the flare. In some cases, hospitalization or surgery may be needed.

