Diet for Gestational Diabetes
Manage blood sugar levels through diet
Medically reviewed by Monique Rainford, MD
Gestational diabetes is high blood sugar (glucose) levels that occur during pregnancy. It affects about 10% of pregnancies in the United States, according to the American Diabetes Association. The good news is that gestational diabetes is treatable.
Food can directly affect blood sugar levels. Because of this, a healthy, balanced diet can help control blood sugar levels and manage gestational diabetes. Learn more about what you can eat to empower yourself to have a safe and healthy pregnancy.
Importance of Managing Blood Sugar
High blood sugar levels can cause complications for both you and your baby during pregnancy, labor, delivery, and after giving birth. It’s crucial to manage blood sugar levels to help decrease the risk of complications and ensure the best possible outcomes for you and your baby.
During the remainder of your pregnancy, you will typically check your blood sugar level multiple times a day, such as in the morning before eating, then after each meal, and before going to bed.
If blood sugar levels are not controlled during pregnancy, you are more likely to give birth to a larger baby, which may result in more severe vaginal tears during vaginal birth, or the need for a cesarean section, as well as heavy bleeding after delivery.
Uncontrolled gestational diabetes can also cause low blood sugar levels in your baby after delivery, which may lead to breathing issues. Your baby also has an increased risk of jaundice (liver issues) and stillbirth when you have gestational diabetes.
Blood Sugar Goals During Pregnancy
Always go by what your healthcare provider has told you, but in general, blood sugar goals during pregnancy are:
Fasting (in the morning before eating): 95 mg/dl or less
One hour after a meal: 140 mg/dl or less
Two hours after a meal: 120 mg/dl or less
Components of Food
Food consists of different macronutrients, including carbohydrates, fat, and protein. These nutrients affect how glucose is digested in our bodies. Read more about each macronutrient to learn how it affects blood sugar levels.
Carbohydrates
Carbohydrates are the main source of energy for your body. They get digested and broken down into molecules called glucose, which is then sent to the bloodstream. Carbohydrates, or glucose, are what increase blood sugar levels.
Carbohydrates are found in many starchy or sugary foods. These includes grains like bread, pasta, rice, oats, and cereal; starchy vegetables like potatoes, peas, and corn; dairy products like milk and yogurt; fruits and fruit juices; and sweets like cookies, cakes, candy, and soda.
Fiber is also a carbohydrate. However, much of the fiber we eat is not fully digested. This means it doesn’t raise blood sugar levels as much as other carbohydrates, making it a healthy choice. Whole grains, fruits, vegetables, and beans all contain fiber.
To help control blood sugar levels, choose more complex carbohydrates with fiber rather than simple carbohydrates like soda, cookies, candy, and other sweets.
Carbohydrates on a Nutrition Facts Label
When managing gestational diabetes, it’s important to know what to look for on a nutrition facts label. Because carbohydrates are what raise your blood sugar levels, you need to pay attention to the total carbohydrates, which are listed in grams. Your healthcare provider or dietitian will let you know how many grams of total carbohydrates you need to eat for meals and snacks.
Underneath the total carbohydrates are dietary fiber, total sugars, and added sugars. Look for foods with three or more grams of fiber and few or no added sugars. You can also look at the ingredients list to see what specific carbohydrates are in the food.
Remember that just because something is listed as sugar-free or "no sugar added" does not mean it is carbohydrate-free. Always base your decision on the total carbohydrate grams when choosing what to include in your meal plan. Pay special attention to serving sizes too, as this will also affect how many grams of carbohydrates are in your meal or snack.
Fat
Dietary fats are important for overall health. Fats provide your body with energy, support cell growth, protect organs, and help keep your body warm. Fats are needed to help absorb some nutrients and produce hormones. Fats also tend to slow down digestion.
The types of fat you eat can make a difference in your health. Saturated and trans fats are less healthy fats and should be limited as much as possible. Saturated fats tend to be solid at room temperature and are found in many animal products, such as meats, dairy, and butter, as well as desserts like cookies, cakes, ice cream, and pastries.
Unsaturated fats are healthier fats and should be included in your diet in moderation. Unsaturated fats tend to be liquid at room temperature and include plant and vegetable oils like olive, avocado, and canola oils. They can also be found in fish, seeds, and nuts.
Protein
Protein is needed to build and repair muscles and other tissues in the body. It also has other important functions, such as to help fight infection, carry nutrients and oxygen throughout the body, contract muscles, balance body fluids, and clot blood.
Protein tends to be digested more slowly than carbohydrates, so combining a meal or snack that has carbohydrates with protein can help prevent blood sugar levels from rising too quickly. Protein is found in both animal and plant-based foods.
Choose lean animal protein and plant-based protein sources, such as poultry without the skin, lean cuts of beef, pork loin, fish, low-fat dairy products, and/or plant-based sources such as legumes, nuts, and seeds. Limiting or eliminating meat and dairy while choosing plant-based protein sources is an overall healthier diet.
Eating Plans
There is no single eating pattern that is best for gestational diabetes. What works for one person might not work for another. Work with your healthcare team to find what works best for you and your lifestyle. Below are some healthy eating patterns that can help manage gestational diabetes.
Verywell / Jessica Olah
DASH Diet
The Dietary Approaches to Stop Hypertension (DASH) diet has been shown to not only help improve blood pressure levels but other health conditions as well, including gestational diabetes.
In a randomized controlled clinical trial of 52 women with gestational diabetes, it was found that consumption of a DASH diet compared with a standard diet for four weeks resulted in improved pregnancy outcomes, including less need for insulin treatment and fewer cesarean sections.
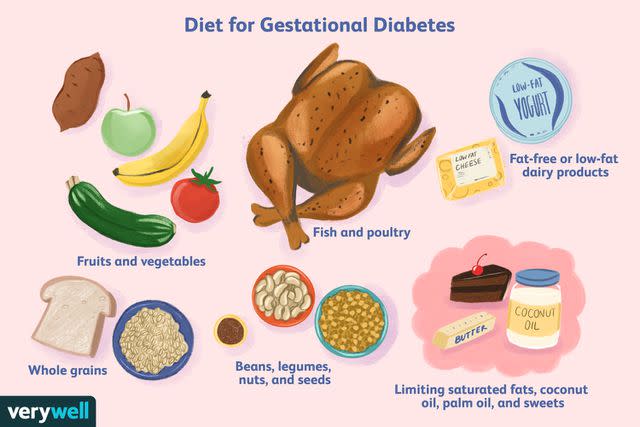
The DASH diet is balanced and flexible to help you create a sustainable, healthy eating pattern for life. This eating plan recommends:
Fruits
Vegetables
Whole grains
Fat-free or low-fat dairy products
Lean proteins, such as fish, poultry, beans, and nuts
Vegetable oils
Limiting foods high in saturated fat, such as fatty meats, full-fat dairy products, and tropical oils such as coconut and palm oils
Limiting sweets and sugar-sweetened beverages
The DASH diet also recommends choosing foods that are low in sodium and saturated and trans fats, while opting for foods higher in fiber, protein, potassium, calcium, and magnesium.
Mediterranean Diet
The Mediterranean diet has been shown to be safe during pregnancy, as well as to reduce the risk of developing gestational diabetes.
Additionally, a study looking at reducing the rate of gestational diabetes found that people who were diagnosed with gestational diabetes had improved gestational outcomes with an early intervention using the Mediterranean diet.
A Mediterranean-style diet typically includes:
Fruits
Vegetables
Beans, legumes, nuts, and seeds
Whole grain bread, pasta, or other whole grains
Olive oil
Fish, and poultry in moderation
Dairy products and eggs
Fish and poultry are more commonly consumed in the Mediterranean diet than red meat. It also emphasizes minimally processed, plant-based foods. Instead of sweets, fruit is frequently eaten for dessert.
Diabetes Plate Method
Another way of eating to help manage gestational diabetes is called the diabetes plate method. The American Diabetes Association suggests this eating plan as a flexible, stress-free way to eat without having to count, calculate, or measure your food.
The diabetes plate method starts with plate size. Using a 9-inch plate, fill half your plate with non-starchy vegetables, such as leafy greens, eggplant, squash, broccoli, Brussels sprouts, or cauliflower. Then fill one quarter with protein foods like lean beef, poultry, fish, eggs, or legumes.
Fill the remaining quarter of your plate with carbohydrate or starchy foods, such as whole-grain bread or pasta, brown or wild rice, potatoes, fruit, yogurt, or milk.
For your beverage, choose water or another zero-calorie drink.
More Eating Tips
Here are more ways to eat healthfully while pregnant, especially when you have gestational diabetes.
Be Consistent With Meals and Snacks
Whichever eating plan you choose to follow, make sure to eat regular meals and snacks. In other words, eat at around the same time each day and about the same amount at each meal and snack. Your body will respond to this consistency, helping your blood sugar levels be more stable in turn.
This might be three regular meals with two or three snacks in between, or it might be five to six small meals throughout the day. Find what works for you, and stick to it.
Related: 12 Healthy Snack Ideas During Pregnancy
Watch Portion Sizes
Portion sizes affect the total carbohydrates in a meal, so it’s important to be mindful of how much you are eating. Carbohydrates should be included in each meal, but don’t overdo it with them.
Depending on the individual, about one cup total of carbohydrate foods per meal is a reasonable portion. This might be different based on your sex, activity level, and blood sugar levels.
Choose Whole Fruit Over Fruit Juice
Fruits contain natural sugars (carbohydrates). Whole fruits also contain dietary fiber. Fruits can be included in your meal plan, but because they contain carbohydrates, you should be mindful of portion sizes, eating only one serving at a time. Generally, a small piece of fruit or one-half cup of fruit or fruit juice counts as a serving size.
Fruit juice counts as fruit, but it usually doesn’t contain the fiber found in whole fruits. For this reason, it’s recommended to choose whole fruit over fruit juice, as the fiber found in whole fruit will help keep your blood sugar levels from rising too high too quickly.
Limit Added Sugars
Carbohydrates are important for our bodies to function properly. Natural sugars are found in foods such as fruits, milk, and yogurt, where they are often accompanied by other nutrients like vitamins and minerals. It’s fine to include these types of sugars in your meal plan, as long as they fit within your carbohydrate goals.
Added sugars are sugars not naturally found in a food. In addition to cakes, cookies, candy, and sugar-sweetened beverages, condiments and other foods often contain added sugars. Even if a food or beverage is sweetened with honey or maple syrup, it is still considered added sugar.
The Dietary Guidelines for Americans recommends little or no added sugars for healthy adults, with a goal of less than 10% of your daily calories coming from added sugars. If you have gestational diabetes, it’s best to limit these types of sugars as much as possible.
Other Treatments for Gestational Diabetes
Besides diet, gestational diabetes is also managed through physical activity and sometimes with medication.
The American College of Obstetricians and Gynecologists (ACOG) says studies have shown that exercise during pregnancy can lower glucose levels in gestational diabetes. Always talk with your healthcare professional before starting a new exercise regimen, but walking is typically a safe form of physical activity for pregnant people.
In addition to diet and exercise, some pregnant people will need medication to help manage their diabetes. This might be an injectable medication, like insulin.
If your practitioner prescribes medication as part of your gestational diabetes treatment plan, be sure to take it as prescribed and report any side effects you notice, such as frequent low blood sugar levels.
When to Call a Healthcare Provider
Call your healthcare provider if you have any of the following:
You are sick and can't get your blood sugar under control
Vomiting or diarrhea for more than six hours
High blood sugar level that stays higher than the level your practitioner has set for you
Low blood sugar level that stays lower than the level your healthcare provider has set for you (for example, 70 mg/dL for two or more readings)
Symptoms of low blood sugar, including:
Sweating
Feeling dizzy, shaky, or weak
Extreme hunger and slight nausea
Headache
Feeling anxious or fast heartbeat
Pale appearance
Confusion
A Word From Verywell
While a diagnosis of gestational diabetes can be disheartening, it does not doom you or your baby to poor pregnancy or delivery outcomes. It is a very treatable condition, especially if you pay attention to your diet and do your best to eat healthfully.
Following a balanced eating pattern during your pregnancy will not only be beneficial for your pregnancy and your baby, but can help you in the postpartum period as well. Work with your healthcare team, including your healthcare provider, dietitian, and/or diabetes educator, to find the eating plan that works best for you.
Read the original article on Verywell Health.

