What Is Deep Vein Thrombosis?
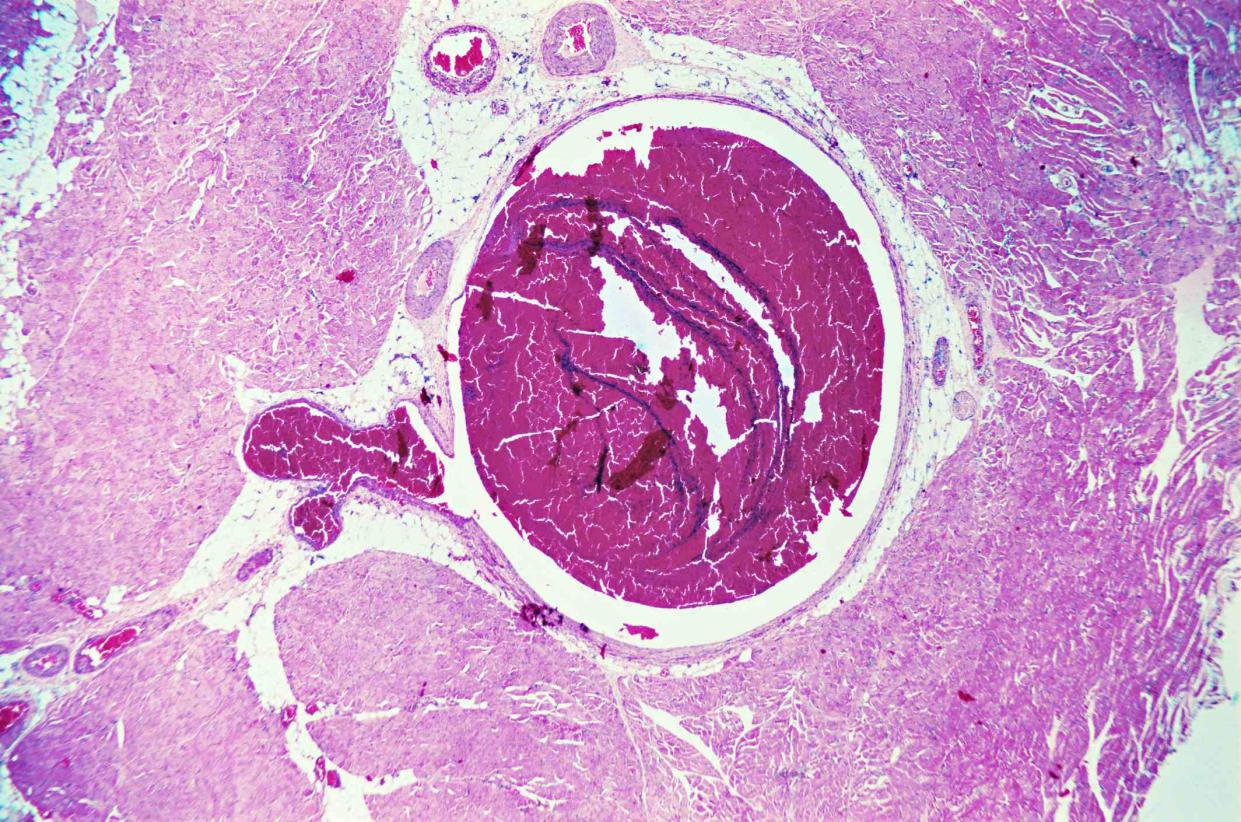
Image Source/Getty images
Medically reviewed by Anisha Shah, MD
Deep vein thrombosis (DVT) is a blood clot that partially or completely blocks a large vein (usually in the lower leg or thigh, like the popliteal vein) though it can occur in other parts of the body.
DVT prevents deoxygenated blood from returning to the heart. As a result, circulation is blocked in the leg, which leads to pain and swelling.
If that blood clot breaks off, it becomes an embolus and can travel through the heart and lungs, blocking passage for blood flow there. A blood clot that travels to your lungs is called pulmonary embolism (PE). PE can deprive the tissues of blood and damage tissues. DVT is very serious and can be fatal.
According to the National Heart, Lung and Blood Institute, blood clots in the thighs are more likely to break off and cause PE than blood clots in the lower leg.
The Centers for Disease Control and Prevention estimates that as many as 900,000 Americans suffer from deep vein thrombosis or PE each year and that 60,000 to 100,000 people die as a result.
It's important to note that DVT is different from a blood clot, which forms in the veins just beneath the skin, known as superficial thrombophlebitis. Superficial thrombophlebitis doesn't usually travel to the lungs and can be treated with anti-inflammatory medications, bed rest, and warm compresses. DVTs are also different from blood clots that occur in the arteries, which can lead to a heart attack or stroke.
Deep Vein Thrombosis Symptoms
Common symptoms of DVT are pain and tenderness in the affected area, and redness or discoloration of the skin. If the DVT breaks off and becomes a PE, you may experience sudden chest pain or chest discomfort that worsens when you take deep breaths, rapid heartbeat, and/or difficulty breathing. Vomiting, coughing up blood, and fainting are also signs of a PE.
DVT and PE are serious, so if you have any of these signs or symptoms, seek help immediately.
Learn More: Symptoms of Pulmonary Embolism
Causes
Adults over age 60 are at the greatest risk for DVT. One of the biggest causes is being immobile and sitting for extended periods of time. Whether you're recovering from surgery or sitting on a long flight, being inactive slows the blood flow and can prevent the platelets and plasma in your blood from mixing and circulating properly.
Other causes of DVT include:
Pregnancy: Women are five times more likely to develop a blood clot when pregnant. A blood clot can happen at any time throughout pregnancy and the first six weeks after giving birth. Increased pressure or injury in the blood vessels in the pelvic area can lead to DVT.
Birth control: Combination hormonal birth control methods (which include both estrogen and progestin) increase the risk of DVT. The risk of developing a clot increases about two-fold when taking the pill and about four-fold when on the patch, vaginal ring, or birth control pills containing desogestrel and drospirenone. However, the overall individual risk is low.
Injury or surgery: Sometimes blood clots that form as part of the healing process may develop into DVT.
Genetic thrombophilia: Some genetic mutations increase the risk of abnormal blood clots. Examples include prothrombin 20210 (also known as factor II) mutation, factor V Leiden thrombophilia, and hereditary antithrombin deficiency (antithrombin III deficiency or AT III deficiency).
Obesity: Increased weight can put pressure on the veins and impair heart function, leading to clots.
Smoking: While research doesn't prove that smoking directly causes DVT, people who smoke are at risk of being overweight or obese, having heart disease and stroke, and developing cancer—all of which are risk factors for DVT.
Diagnosis
If you have a DVT, it's important to get diagnosed right away before it becomes a pulmonary embolism. Once a PE blocks an artery in your lung, all blood flow is reduced or stopped completely, which can cause sudden death.
Your healthcare provider will most likely perform a compression ultrasound, but other tests, like a venogram, CT scan, or D-dimer test, can also be used to diagnose DVT. Through a compression ultrasound, your practitioner is able to see the blood clot and the obstruction of blood flow in the vein.
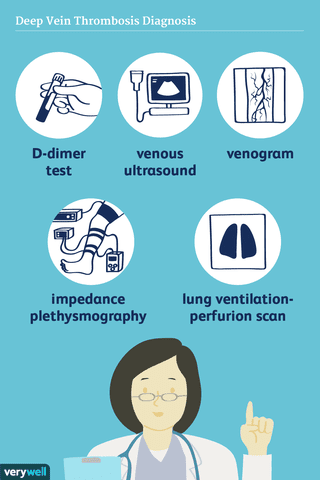
Verywell
Learn More: How Deep Vein Thrombosis Is Diagnosed
Treatment
If your healthcare provider confirms a DVT diagnosis, the first line of treatment is usually anticoagulants (blood thinners). Anticoagulants do not break up existing clots, but work to prevent further blood clotting in the veins and reduce your chances of developing a PE. There are injectable and pill forms of anticoagulants.
If you do develop a PE and have a large clot, you may be prescribed thrombolytic therapy (clot-busting medication). These medications are given through IV or a catheter injected directly into the clot. Clot busting medications are typically reserved for emergency cases due to the risk for severe bleeding.
Guidelines for DVT and PE
Treatment guidelines have been updated to conditionally recommend that certain people with DVT or PE with a low risk of complications can be treated at home instead of the hospital.
Once short-term treatment is done, your healthcare provider may put you on another anticoagulant. Anticoagulation therapy usually continues for three months, but in some cases, it can be indefinite, especially if you've had a PE. Your practitioner will evaluate your case against the risks and benefits as part of their clinical decision-making.
In 2020, the American Society of Hematology (ASH) released updated treatment guidelines for DVT and PE. Updates to these evidence-based treatment recommendations to be aware of include:
For people with PE and cardiac instability, clot-busting medications (thrombolytic therapy) followed by anticoagulation is recommended over just anticoagulation alone.
For patients with recurrent unprovoked DVT or PE, continuing anticoagulation therapy indefinitely is recommended rather than stopping anticoagulation after primary treatment.
Learn More: How Deep Vein Thrombosis Is Treated
Prevention
It's important for people at risk of DVT, or those who have had one, to maintain a healthy lifestyle. Quitting smoking, achieving a healthy weight, and following a regular exercise routine are all helpful prevention strategies.
You should avoid sitting for long periods of time and stretch and move throughout the day. Compression socks are especially helpful on long flights because they aid in circulation and help the leg veins return deoxygenated blood to the heart.
If you're taking birth control or hormone replacement therapy, you can talk to your healthcare provider about changing your treatment plan to prevent future clots. People who have hypertension, heart disease, or heart failure are also at a high risk of DVT, so be sure to talk with your healthcare provider about creating a treatment plan that lowers your risk and prevents clots.
Learn More: Prevention of Deep Vein Thrombosis
Summary
Deep vein thrombosis is a serious condition that should be treated immediately. It usually takes three to six months for the clot to completely resolve, but through medical treatment, you can prevent the clot from increasing in size and breaking away.
If you experience symptoms of pulmonary embolism, get help right away. While the symptoms of DVT can be alarming, knowing them can help save your life or someone you know.
Read Next: Symptoms of Deep Vein Thrombosis

