After COVID-19, our next big health care challenge will be drug-resistant infections
Data by Johns Hopkins University and the Centers for Disease Control and Prevention shows that COVID-19 deaths approached the 1 million mark Thursday. To mark the "tragic milestone," President Joe Biden directed flags on government buildings to be flown at half-staff for five days.
COVID-19 reminded us of what the world looked like without the right diagnostics, treatments or vaccines for just one virus. Now, imagine if most of the medicines we rely on today for the most common illnesses – strep throat, sinus infections or urinary tract infections – became ineffective.
These illnesses could become life-threatening occurrences.
Many surgeries would be too risky to perform because infections could be unstoppable and interacting with each other would become untenable.
COVID-19 isn't the only threat to public health
Unfortunately, this reality is already here and worsening, and if not addressed, it will pose the most significant health threat to humanity. It’s called “antimicrobial resistance” (AMR) – known to many of us as “antibiotic resistance” – and it occurs when microorganisms such as bacteria, viruses, parasites and fungi evolve and adapt in a way that renders ineffective the medications previously designed to stop them.
Overturning Roe: Meet the women working to overturn Roe v. Wade and restrict abortions across America
These microorganisms become “superbugs.” The overuse of antibiotics by people and animals is fueling resistance – shortening the lifespans and effectiveness of our medicines and causing a dramatic increase in the cost of combating routine infectious diseases.
The U.S. Centers for Disease Control and Prevention (CDC) estimates that drug-resistant infections kill 35,000 Americans each year and contribute to 2.8 million illnesses.
And the World Health Organization reports 700,000 annual deaths worldwide, with the problem projected by British economist Jim O'Neill to grow to 10 million deaths by 2050.
By comparison, consider that more than 6 million people worldwide have died from COVID-19 over a two-year period.
They didn't find any CRT: Delaware HBCU team’s bus searched in Georgia
As an anesthesiologist and critical care doctor who has been on the front line of public health through disease outbreaks such as Ebola, Zika and COVID-19, I have had a front-row seat to some of the most severe consequences of AMR while in the operating room. I have seen my patients die after a seemingly successful surgery because the bacterial infection in their body had become resistant to all our medicines.
Truth be told, we may not be able to fully stop AMR. For example, based on its own data, the CDC estimates that half of gonorrhea infections, which increased during the pandemic, were resistant to at least one antibiotic. However, we can drastically reduce AMR’s progression if we recognize the threat and take comprehensive action. How we manage the use of antibiotics in the years to come will determine the impact of this crisis on each and every one of us.
While antibiotics in many ways are a medical miracle that should be preserved, we must use them with the utmost care and stewardship. Americans consume more than 260 million courses of antibiotics each year, and yet the CDC estimates that as many as 50% of all antibiotics prescribed in the United States are not medically necessary.
Prioritize the development of new antibiotics
So how do we address this problem? For starters, policymakers and innovators must prioritize the development of new antibiotics. At the same time, they must take steps to slow the progression of AMR to buy the requisite time needed to develop novel anti-infective agents. All the stakeholders in the medical supply chains, ranging from drug and diagnostics manufacturers, distributors and prescribers, and patients themselves, must recognize the gravity of this situation. The household discussions around AMR must become as commonplace as COVID-19 is today.
Fixing the formula shortage: Let's not waste time placing blame over baby formula shortage
One way to maximize our ability to manage AMR is by focusing on point-of-care diagnostic testing to support antibiotic stewardship. If we are going to dramatically reduce the use of medically unnecessary antibiotics, we must give our front-line clinicians the fast, accurate tools they need to differentiate between viral and bacterial infections and determine when antibiotics will be effective.
My family was recently confronted with this problem when my daughter became ill. I had just finished my tenure as U.S. surgeon general, and I was unable to distinguish whether her infection, if not COVID-19, was viral or bacterial, or merely allergies, because all three can cause similar symptoms. Without definitive answers, her care and our response as a family were uncertain, as her prognosis impacted whether she and her siblings should return to school.
The United States has already begun setting the building blocks for success. Congress is considering incentivizing new investments in antibiotic development. The CDC has formed a National Action Plan and partnered with states, like Florida, to track AMR and educate health care providers and the public of the problem.
Mental health as a priority: It's time to demand timely mental health reporting by colleges and universities
And, earlier this year, the Biden administration launched a new Test to Treat Initiative, which will help health care providers quickly differentiate between COVID-19 (a viral infection) and other bacteria-caused illnesses, cutting down on the use of unnecessary antibiotics. This initiative follows examples set by countries like the United Kingdom that have implemented rapid tests and defined treatment paths in their local pharmacies to improve access and efficiency.
Now is the time to expand our front-line AMR response and give primary care doctors, nurses, pharmacists and their patients the tools they need to practice antibiotic stewardship. This will significantly prolong the effectiveness of the antibiotics we have and give us the time to enable the development of the next generation of antibiotics.
One lesson that we all have learned from the COVID-19 pandemic is that there simply is no substitute for effective rapid testing and early treatment at the point of care. The next major health crisis has already begun, and how we take action to address it will determine how it impacts our children and grandchildren.
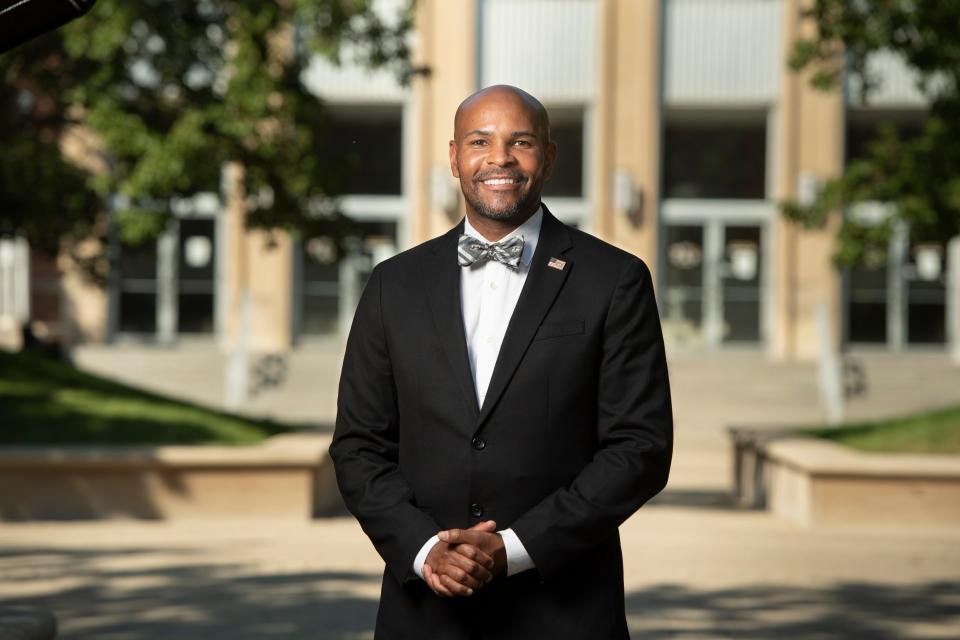
Dr. Jerome Adams, a former U.S. surgeon general, is a distinguished professor and executive director of health equity initiatives at Purdue University. Follow him on Twitter: @JeromeAdamsMD
You can read diverse opinions from our Board of Contributors and other writers on the Opinion front page, on Twitter @usatodayopinion and in our daily Opinion newsletter. To respond to a column, submit a comment to letters@usatoday.com.
This article originally appeared on USA TODAY: After COVID ends, antimicrobial-resistant bugs pose a new challenge

