Causes and Treatment of Itching in Dialysis Patients
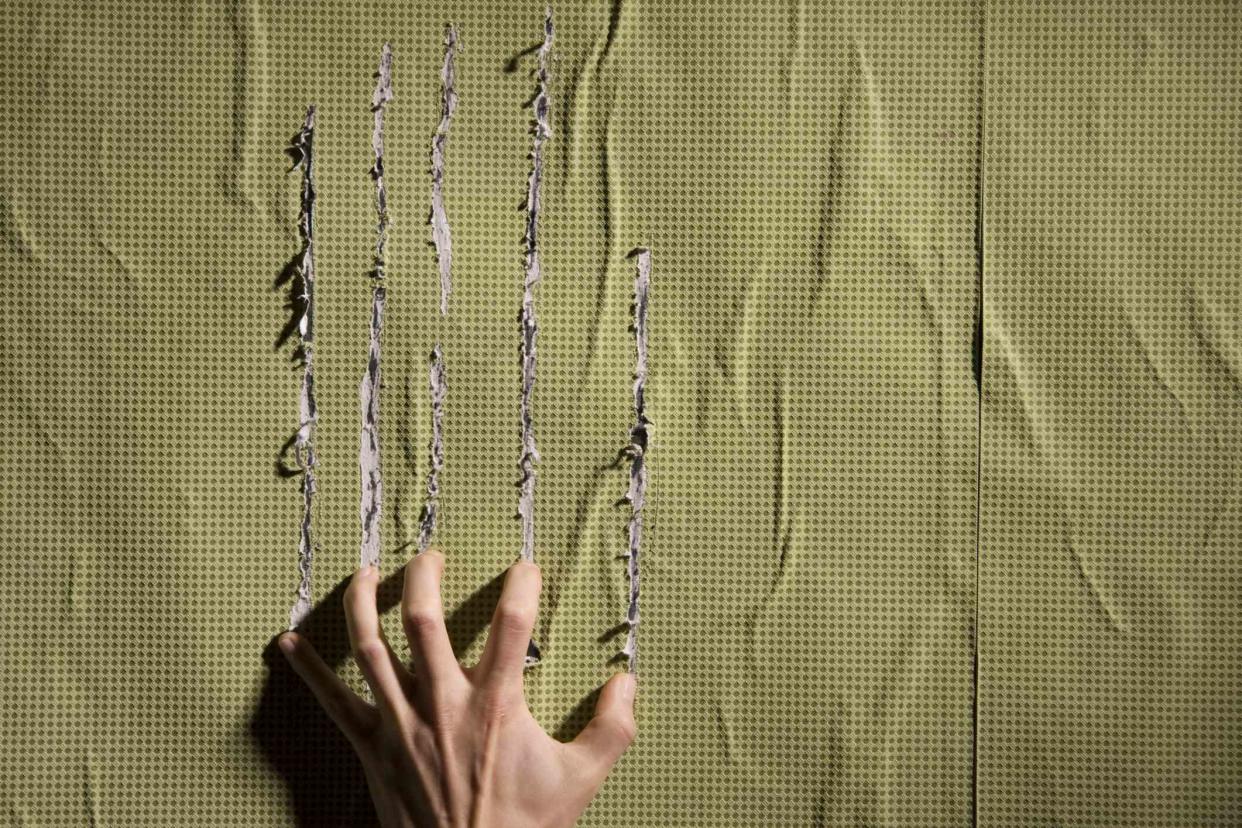
sodapix / Getty Images
Medically reviewed by Jamin Brahmbhatt, MDFact checked by Nick Blackmer
Pruritus, or as normal people call it, itching, is a common problem that afflicts patients with kidney failure or dialysis patients. It is one of those complications of advanced kidney disease that is hard to understand and perhaps harder to treat.

How Common Is Itching In Dialysis Patients?
One of the major studies to address this question reported in 2006 that itching was experienced by close to half of dialysis patients. This data was gathered from patients on hemodialysis, but we still don't have a good idea of what proportion of patients with advanced kidney disease who are not yet on dialysis, or even patients on peritoneal dialysis, have this problem.
Why It Happens
This is not completely understood. Here are a few possibilities that we know of:
One speculation is that since dialysis is a state where the body is in a state of chronic inflammation, this might be an inflammatory disorder. There have been studies that have looked at so-called "markers of inflammation" which have been shown to be high in patients with kidney failure experiencing pruritus.
Dry skin is a common problem in dialysis patients which could be a contributing factor.
Other allergy related and neurological causes have also been blamed for this.
Symptoms
Well, you itch. But here are a few specific points:
Itching tends to be worse at night to the point where it can disturb sleep.
It tends to commonly affect the back although the rest of the body is not necessarily off limits.
Heat seems to make it worse.
Does It Affect Every Dialysis Patient?
Not necessarily. However, there are patients in whom certain risk factors have been identified. This is not a complete list since this is an active area of research:
Lack of adequate dialysis is a major risk factor. Patients who do not receive active adequate dialysis tend to be more "uremic." Itching tends to be worse in that situation.
It also seems to be associated with high levels of phosphorus in the blood although other lab abnormalities including high magnesium and aluminum concentrations have all been blamed.
Finally, dialysis patients tend to have high levels of parathyroid hormone, which is part of an entity called chronic kidney disease related mineral and bone disorder. These patients are also seen to be higher risk.
Treatment
Identifying the underlying risk factor that might be a cause is the really the first step. If the patient who is not being adequately dialyzed or is missing treatments complains of itching, then the initial "treatment" would probably be prescribing an optimal dose of dialysis, rather than starting the patient on any specific medication for itching. One of the ways of increasing the dose of dialysis is to increase the duration of the treatment. This, however, may or may not be an acceptable option to a patient. Other interventions that can be tried to make sure patients are getting an efficient treatment is to increase their blood flow rates during the treatment, or making sure that they have a good dialysis access where ideally no recirculation is going on.
If the above steps are already in place or if the dose of dialysis does not seem to be an issue, then the nephrologist needs to look at your lab tests. Is the parathyroid hormone (PTH) or your phosphorus high? If these or other risk factors are easily identifiable, steps can be taken to fix that. For instance, vitamin D analogs can help bring down that PTH level. High phosphorus levels could be brought down by a low phosphorus diet or by putting patients on phosphorus binders.
Finally, if all this fails, we often have to turn to medications. These could include an antihistamine like Benadryl or diphenhydramine, or another medication which is similar called hydroxyzine. These medications will tend to be sedating and may not work in all cases. Loratadine is a non-sedating alternative.
Other medications that have been tried include gabapentin, pregabalin, and antidepressants including sertraline. For patients who get no relief even with these drugs, phototherapy with ultraviolet B light might help.
