What Causes Secondary Osteoarthritis?
Some conditions are risk factors for developing OA
Medically reviewed by Riteesha G. Reddy, MD
Osteoarthritis (OA) results from the gradual wearing down of the protective cartilage cushioning the ends of bones. OA can be either primary or secondary. Primary OA is primarily related to aging, whereas secondary OA is osteoarthritis caused by another disease or condition.
Examples of conditions leading to secondary OA include repeated trauma or surgery to a joint structure, congenital abnormalities (joint conditions at birth), inflammatory arthritis, and metabolic disorders. Secondary OA can affect young and old alike.
This article discusses what conditions cause secondary OA and what it feels like. It also covers how it's diagnosed and treated and what you can do to prevent it.
Secondary Osteoarthritis Symptoms
Both primary and secondary OA involve the breakdown of joint cartilage, which causes bones to rub together, called bone-on-bone pain. The most common symptom caused by OA is pain in the affected joints, especially after repetitive use.
Symptoms in OA tend to occur slowly and affect one or more joints. However, early on, OA might not cause symptoms.
When symptoms of secondary OA do appear, you may experience:
Joint swelling and stiffness
Loss of range of motion (difficulty moving affected joints)
Pain that worsens with inactivity
Warmth and tenderness in affected joints
Loss of muscle mass
Crepitus—grating or cracking sounds in the joints
Secondary OA may progress over time, especially if it causes inflammation.
When osteoarthritis is secondary to a type of autoimmune arthritis, such as rheumatoid arthritis (RA), synovitis—mild inflammation of the soft tissues around the joints—is common.
Additional signs of progression in OA are:
Cartilage that has worn away
Reduced spacing between joints
Warm and inflamed joints
Reduction of normal joint lubricating fluid
Bony growths and bone rubbing against bone
If your OA has advanced, you will have pain and discomfort when moving affected joints. The pain is often severe enough that it keeps you from performing day-to-day activities.
Related: Signs and Symptoms of Osteoarthritis
What Conditions Cause Secondary Osteoarthritis?
Unlike primary OA, secondary OA has a specific cause. It also occurs in younger people, usually those under 35 years of age.
The following are primary conditions that are risk factors associated with secondary OA.
Joint Injuries
Repetitive bone fractures increase a person’s chance of developing OA. This can also bring about early onset of the disease. This is common in people who repeatedly stress one joint or a group of joints, such as in certain occupations. In fact, occupation is a major risk factor for knee osteoarthritis, especially in jobs where repetitive knee bending is required.
Congenital Joint Deformities
Sometimes, a person is born with abnormally formed joints—called congenital abnormalities—that are vulnerable to injury, joint cartilage loss, and early degeneration.
An example of a congenital joint deformity condition is congenital hip dysplasia. This occurs when the hip socket doesn’t fully cover the ball part of the upper thighbone, causing the hip joint to become either partially or completely dislocated. A person with hip dysplasia may develop severe osteoarthritis in their hip later in life.
Autoimmune Inflammatory Arthritis
Some diseases cause inflammation in the affected cartilage, eventually damaging the joints and leading to osteoarthritis. One such condition is rheumatoid arthritis (RA).
Rheumatoid arthritis is most commonly associated with secondary OA. RA is an autoimmune disease that can affect more than just a person’s joints. In some people, it also affects other body systems, including the heart, lungs, blood vessels, skin, and eyes.
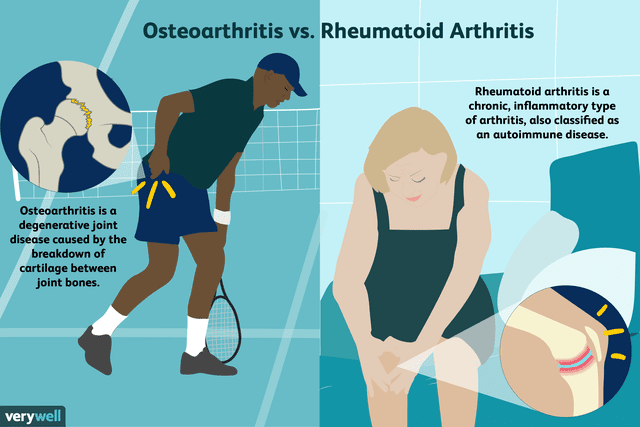
Being an autoimmune disease, rheumatoid arthritis occurs when the immune system mistakenly attacks its own body’s healthy tissues. Its connection to secondary OA starts when RA causes inflammation to the synovium—the soft tissue lining the joints—eventually damaging the cartilage and reducing joint stability.
In 2015, a study published in Annals of the Rheumatic Diseases found a high prevalence of secondary OA of the knee in people with rheumatoid arthritis.
Here, the researchers reviewed medical histories of 565 patients with rheumatoid arthritis in a rheumatology clinic setting. They looked at the disease symptoms, medical history, physical examinations, and results of ultrasound and X-ray imaging. The researchers eventually determined that 71% of the study participants had secondary OA of the knee, which was more common with increased activity, morning stiffness, and the longer a person had rheumatoid arthritis.
In 2017, a study published in the journal Arthritis & Cartilage described that secondary OA appeared to be a bigger problem than inflammation in patients with RA. The authors also mentioned it was possible that RA could be worse in people with secondary OA. The authors suggested that doctors should consider measurements of joint damage and distress as they make clinical decisions for their patients.
Diseases of Cartilage or Bone
Any number of conditions affecting the structure of cartilage or bone may trigger secondary osteoarthritis. This can include acromegaly and Paget’s disease.
Acromegaly causes excessive secretion of human growth hormone, resulting in a gradual increase in the head, face, hands, feet, and/or organs. Bone and cartilage problems, inflammation, and gradual degeneration from acromegaly may eventually result in osteoarthritis.
Paget’s disease, a condition disrupting normal bone formation, causes bones to be weak and become deformed over time. According to the National Institutes of Health, people with Paget’s disease frequently have osteoarthritis as well. Paget’s disease causes OA if it changes the shape of bones, causes long bones to bow and bend, places stress on the joints, changes the curvature of the spine, and/or softens the pelvis, which reduces the stability of the hip joints.
Metabolic disorders
Metabolic disorders are the result of abnormal chemical reactions in the body that modify the normal metabolic process. In 2016, a study was published in the Journal of Orthopaedics that reported on an earlier published National Health and Nutrition Examination (NHANE) analysis, finding that 59% of the population has metabolic syndrome along with OA.
Examples of metabolic disorders associated with OA include hypertension and diabetes mellitus. Too much iron in the body due to a condition called hemochromatosis is another metabolic condition that can predispose a patient to OA in common joints such as the knees. It may also affect joints that are not commonly affected with primary OA, such as the large knuckles of the hand (MCP joints), shoulders, or ankles.
Diagnosing Osteoarthritis
Whether or not a person has primary or secondary OA, the diagnosis process remains the same. Testing for OA may include:
Blood work: There is no specific blood test that can diagnose OA, but blood tests are done to rule out conditions that cause secondary OA and other arthritic conditions that may mimic OA.
X-rays: X-rays of affected joints are helpful in diagnosing OA. X-ray findings associated with OA show loss of joint cartilage, joint space narrowing between the nearby joints, and bone spurs. X-rays can also exclude other causes of your pain and help your healthcare provider determine whether you may need surgery.
Magnetic resonance imaging (MRI): MRI uses radio waves and a strong magnetic field to produce detailed images of the bone, cartilage, and other soft tissues. MRI scanning is utilized to diagnose OA in more serious cases.
Arthrocentesis: Often done in your healthcare provider’s office, this procedure involves the use of a sterile needle to remove joint fluid for analysis. Joint fluid analysis can diagnose or rule out inflammatory arthritis. The removal of joint fluid may also help relieve pain, swelling, and inflammation.
Arthroscopy: If your healthcare provider finds or suspects you might have joint or cartilage damage, an arthroscopy may be performed. This involves inserting a tube with a small camera attached to it to look into the joint space for abnormalities and cartilage damage. It is possible to repair some of the damage during this procedure, and most people who have arthroscopic surgery usually recover quicker than those who have open joint surgery.
Takeaway
Your healthcare provider will also want to carefully analyze the appearance, location, extent, and duration of joint symptoms.
Bony formations in the joints are characteristic of osteoarthritis. Additionally, nodes—either Bouchard’s nodes, Heberden’s nodes, or both—in the fingers and bunions on the feet can also help in diagnosing OA.
Related: Differential Diagnosis of Osteoarthritis
Secondary Osteoarthritis Treatment
Treatment for secondary OA begins with managing the underlying cause and getting it under control. Your healthcare provider will focus on treating your OA, and treatment is dependent on symptoms, severity, and personal preferences or needs.
Treatment usually starts with simple and noninvasive therapies. You will need more intensive treatment if symptoms aren’t manageable with over-the-counter treatments and lifestyle changes. Some people may need physical therapy, stronger pain relievers, and surgery to manage severe OA.
Over-the-Counter Pain Relievers
Several types of OTC medications can help in relieving OA symptoms. Tylenol (acetaminophen) is an OTC pain reliever. While it can help reduce pain, it does not help with inflammation, and taking too much can cause liver damage.
Nonsteroidal anti-inflammatory drugs (NSAIDs) can help with multiple OA symptoms, including pain and inflammation. OTC NSAIDS include aspirin, ibuprofen, and naproxen.
Talk to your healthcare provider about whether it is safe for you to take OTC NSAIDs, because they are known for significant side effects such as stomach problems, cardiovascular diseases, bleeding problems, and liver or kidney damage. Using a topical NSAID (applied to the skin) may reduce the risk of side effects.
Lifestyle Changes
Many people can control OA symptoms with basic lifestyle changes. This can include losing weight, staying active, not smoking, resting when joints are swollen and hurting, and using hot and cold therapy to relieve pain and swelling. Talk to your healthcare provider about what lifestyle changes might be best for your unique situation.
Prescription Treatments
Sometimes, OTC pain relievers aren’t enough to reduce pain and swelling or improve the quality of life. In this case, your healthcare provider may prescribe stronger medicines to manage symptoms.
Corticosteroids can help reduce inflammation, which improves pain and swelling. With OA, corticosteroids are usually given by injection and administered by your healthcare provider or nurse.
Your healthcare provider can also prescribe a stronger NSAID to reduce pain. Prescription NSAIDs are available in stronger doses and work for longer periods. Both corticosteroids and NSAIDs cause harsh side effects. Talk to your practitioner about the best ways to reduce the risk of NSAID side effects.
Physical Therapy
Physical therapy can be useful for managing OA. It can help with strengthening muscles, increasing range of motion, reducing joint pain and stiffness, and improving balance and gait. A physical therapist can also recommend assistive devices—such as braces, splints, a cane or walker—to provide support for weakened joints, take the pressure off the injured joints, and reduce pain.
Surgery
Severe cases of OA may require surgery to replace or repair damaged joints. There are several surgery types, including joint replacement, bone realignment, bone fusion, and arthroscopic surgery.
Takeaway
There are many options available to you for treating OA. Work with your healthcare provider to find the right treatments for your unique situation.
Related: How Osteoarthritis Is Treated
Preventing Secondary Osteoarthritis
There is a lot you can do to prevent secondary OA. One of the main ways is by managing risk factors for the condition. This includes managing any condition that increases your risk for secondary OA. A healthy lifestyle can also reduce the risk of developing secondary OA.
For example, diabetes can be a significant risk factor for OA, according to the Arthritis Foundation. High glucose levels may speed up the process that increases the stiffness of the cartilage. Also, diabetes may trigger inflammation, which also speeds up cartilage loss. Keeping diabetes under control and regulating sugar levels can prevent OA.
Takeaway
Making certain lifestyle changes can help improve joint health and prevent OA.
Maintaining a healthy lifestyle includes getting plenty of rest and enough sleep, keeping a healthy diet and managing weight, not smoking, and only drinking alcohol in moderation.
Outlook for Secondary Osteoarthritis
The prognosis for secondary osteoarthritis depends on the joints affected and how severe OA is. There are currently no disease-modifying treatments available that could reduce the effects of secondary OA. That means treatment is directed at managing pain and other OA symptoms and managing the underlying condition. With treatment, the outlook for OA is positive in reducing symptoms.
Summary
Secondary osteoarthritis happens when your cartilage wears down in the joints due to another condition. Causes may include joint injuries, congenital joint deformities, and rheumatoid arthritis. Secondary OA is diagnosed with tests including blood work, X-rays, MRI, arthrocentesis, and arthroscopy.
Managing secondary OA involves treating the underlying condition. To help relieve symptoms, your healthcare provider may recommend OTC pain relievers, such as aspirin and ibuprofen, and healthy lifestyle changes. If needed, your healthcare provider can prescribe treatments such as corticosteroids to reduce inflammation.
Read the original article on Verywell Health.

