Cancer Cells vs. Normal Cells: How Are They Different?
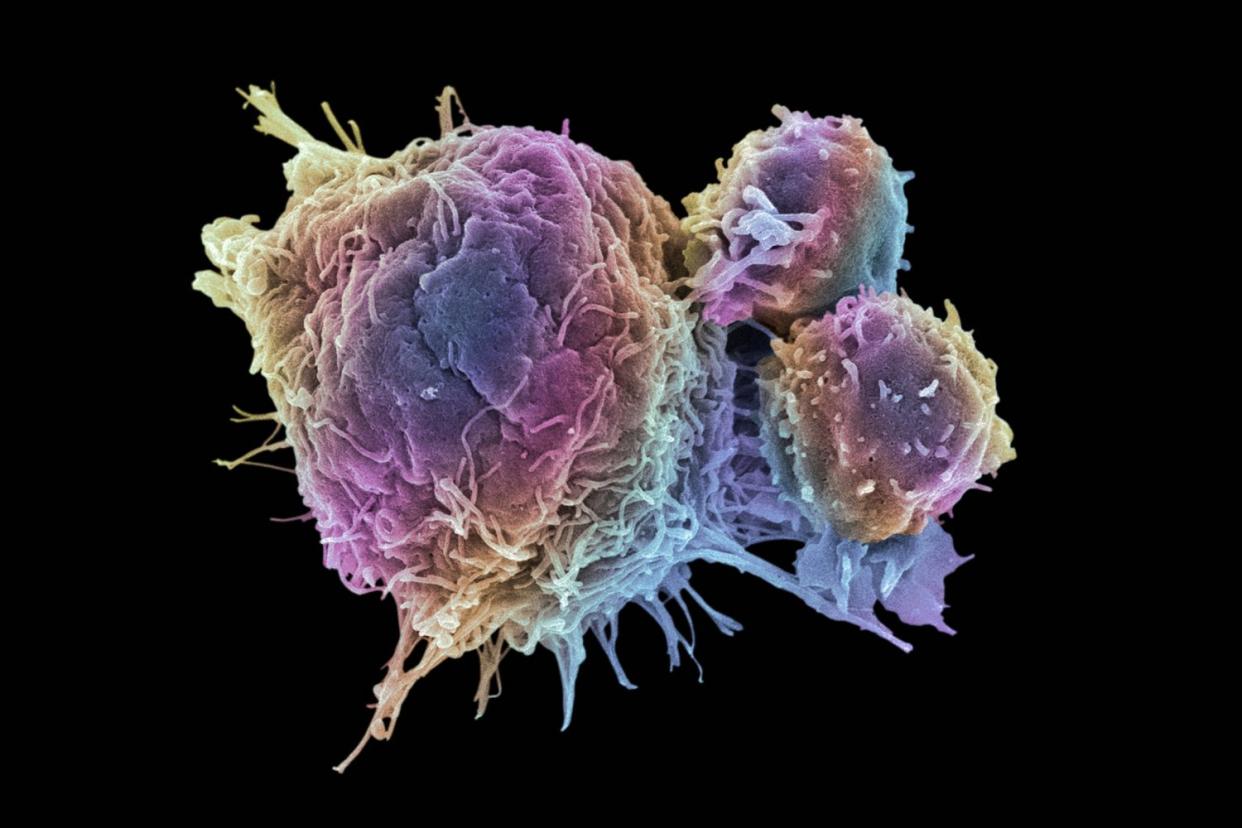
Steve Gschmeissner/Science Photo Library/Getty Images
Medically reviewed by Doru Paul, MD
Cancer cells are different from normal cells in how they grow, how they look, and what they do in the body. Even though cancer is common, there are actually many steps that a normal cell has to go through to become a cancerous cell.
This article will explain how cancer cells and normal, healthy cells are different. It covers the basic differences between cancer cells and normal cells, like how they grow and communicate. It also goes a bit deeper, covering technical differences between normal cells and cancer cells, including how they invade tissue in the body and "hide" from cancer treatments.
Related:How Common Is Cancer?
Basic Differences Between Cancer Cells and Normal Cells
There are many differences between cancer cells and normal cells in noncancerous (benign) or cancerous (malignant) tumors.
The major differences between normal cells and cancer cells relate to growth, communication, cell repair and death, "stickiness" and spread, appearance, maturation, evasion of the immune system, function and blood supply.
| Normal Cells | Cancerous Cells |
Growth | Stop when there's enough | Uncontrolled growth |
Communication | Respond to signals from other cells | Do not respond to signals from other cells |
Cell repair/death | Aged/damaged cells are repaired or replaced | Cells are neither repaired or replaced |
Stickiness/spread | Stay together in assigned area | Can travel solo and throughout the body |
Appearance | Uniform look under a microscope | Varied sizes, larger and darker center under a microscope |
Maturation | Reach maturity | Do not reach maturity |
Evasion of immune system | Can be targeted and eliminated | Can "hide" and grow uninterruputed |
Function | Perform designated tasks | Fail to perform designated tasks |
Blood supply | Blood vessels grow to feed normal growth and aid in repairs | Blood vessels grow regardless, constantly "feeding" a tumor |
It's these differences that account for how cancerous tumors grow and respond differently to their surroundings than benign tumors.
Growth
Normal cells stop growing (reproducing) when enough cells are present. For example, if cells are being produced to repair a cut in the skin, new cells are no longer produced when there are enough cells present to fill the hole (when the repair work is done).
In contrast, cancer cells don’t stop growing when there are enough cells present. Cancer cells reproduce rapidly before they have had a chance to mature. This continued replication often results in a tumor (a cluster of cancer cells) being formed.
Each gene in the body carries a blueprint that codes for a different protein. Some of these proteins are growth factors—chemicals that tell cells to grow and divide.
If the gene that codes for one of these proteins is stuck in the “on” position by a mutation (an oncogene) the growth factor proteins continue to be produced. In response, the cells continue to grow.
This video has been medically reviewed by Doru Paul, MD
Related:How Do Oncogenes Cause Cancer?
Communication
Cancer cells don’t interact with other cells as normal cells do. Normal cells respond to signals sent from other nearby cells that say, “you’ve reached your boundary.” When normal cells “hear” these signals they stop growing. Cancer cells do not respond to these signals.
Cell Repair and Cell Death (Homeostasis)
Homeostasis is the body's way of ensuring all its processes are working properly. Homeostasis is one area where normal cells and cancer cells are very different.
To maintain homeostasis, normal cells are either repaired or die (undergo apoptosis) when they are damaged or get old. Cancer cells are either not repaired or do not undergo apoptosis.
For example, one protein called p53 has the job of checking to see if a cell is too damaged to repair, and if so, advise the cell to kill itself. If this protein p53 is abnormal or inactive (for example, from a mutation in the p53 gene), then old or damaged cells are allowed to reproduce.
The p53 gene is one type of tumor suppressor gene that code for proteins that suppress the growth of cells.
Related:What Are Tumor Suppressor Genes?
Stickiness
Normal cells secrete substances that make them stick together in a group. Cancer cells fail to make these substances, and can “float away” to locations nearby, or through the bloodstream or system of lymph channels to distant regions in the body.
Spread
Normal cells stay in the area of the body where they belong. For example, lung cells remain in the lungs. Some cancer cells may lack the adhesion molecules that cause stickiness, and are able to detach and travel via the bloodstream and lymphatic system to other regions of the body—they have the ability to spread (metastasize).
Once they arrive in a new region (such as lymph nodes, the lungs, the liver, or the bones) they begin to grow, often forming tumors far removed from the original tumor.
Related:How Cancer Spreads
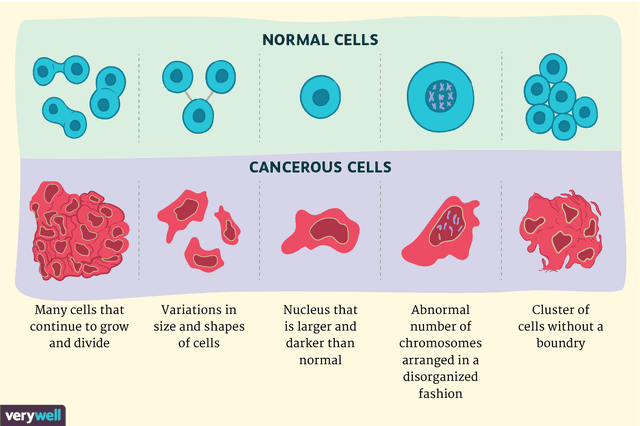
Appearance
Under a microscope, normal cells and cancer cells may look quite different. In contrast to normal cells, cancer cells often exhibit much more variability in cell size—some are larger than normal and some are smaller than normal.
In addition, cancer cells often have an abnormal shape—both the cell and the nucleus (the “brain” of the cell.) The nucleus appears both larger and darker than normal cells.
The reason for the darkness is that the nucleus of cancer cells contains excess DNA. Up close, cancer cells often have an abnormal number of chromosomes that are arranged in a disorganized fashion.
Maturation
Normal cells mature. Cancer cells, because they grow rapidly and divide before cells are fully mature, remain immature. Doctors use the term undifferentiated to describe immature cells (in contrast to differentiated to describe more mature cells.)
Another way to explain this is to view cancer cells as cells that don’t “grow up” and specialize to adult cells. The degree of maturation of cells corresponds to the grade of cancer. Cancers are graded on a scale from 1 to 3 with 3 being the most aggressive.
Related:How Are Cancer Tumors Graded?
Evasion of the Immune System
When normal cells become damaged, the immune system (via cells called lymphocytes) identifies and removes them.
Cancer cells are able to evade (trick) the immune system long enough to grow into a tumor by either escaping detection or by secreting chemicals that inactivate immune cells that come to the scene. Some of the newer immunotherapy medications address this aspect of cancer cells.
Function
Normal cells perform the function they are meant to perform, whereas cancer cells may not be functional.
For example, normal white blood cells help fight off infections. In leukemia, the number of white blood cells may be very high, but since the cancerous white blood cells are not functioning as they should, people can be more at risk for infection even with an elevated white blood cell count.
The same can be true of substances produced. For example, normal thyroid cells produce thyroid hormones. Cancerous thyroid cells (thyroid cancer) may not produce thyroid hormone. In this case, the body may lack enough thyroid hormone (hypothyroidism) despite an increased amount of thyroid tissue.
Blood Supply
Angiogenesis is the process by which cells attract blood vessels to grow and feed the tissue. Normal cells undergo a process called angiogenesis only as part of normal growth and development and when new tissue is needed to repair damaged tissue.
Cancer cells undergo angiogenesis even when growth is not necessary. One type of cancer treatment involves the use of angiogenesis inhibitors—medications that block angiogenesis in the body in an effort to keep tumors from growing.
Related:Why Do Cells Turn Into Cancer?
How Do Cells Become Cancerous?
There are proteins in the body that regulate cell growth. Your DNA carries genes that are the blueprint for proteins produced in the body.
Some of these proteins are growth factors—chemicals that tell cells to divide and grow. Other proteins work to stop (suppress) growth.
Mutations in particular genes—for example, those caused by tobacco smoke, radiation, ultraviolet radiation, and other carcinogens—can result in the abnormal production of proteins. Too many might be produced or not enough. Sometimes, the proteins are abnormal and function differently.
Normally, roughly three billion cells divide in the body every single day. When “accidents” in the reproduction of these cells happen during any of those divisions (for example, caused by genes or environmental carcinogens), it may create a cell that can mutate more and develop into a cancer cell.
That said, there are several “checkpoints” that need to be bypassed for a cell to become cancerous:
The cell needs to have growth factors that prompt it to grow even when growth is not necessary.
The cells have to evade proteins that direct cells to stop growing and die when they become abnormal.
The cell needs to evade signals from other cells,
The cells need to lose the normal “stickiness” (adhesion molecules) that normal cells produce.
It takes a combination of abnormalities to make a cancerous cell happen, rather than a single mutation or protein abnormality. It's actually very difficult for a normal cell to become cancerous, which may seem surprising considering that one in three people will develop cancer in their lifetime.
Related:Cancer Growth and Angiogenesis
A Deeper Dive Into the Technical Differences
This list contains further differences between healthy cells and cancer cells.
Evading Growth Suppressors
Normal cells are controlled by growth (tumor) suppressors. There are three main types of tumor suppressor genes that code for proteins that suppress growth.
One type tells cells to slow down and stop dividing.
Another type is responsible for fixing changes in damaged cells.
A third type is in charge of the apoptosis noted above.
Mutations that result in any of these tumor suppressor genes being inactivated allow cancer cells to grow unchecked.
Invasiveness
Normal cells listen to signals from neighboring cells and stop growing when they encroach on nearby tissues (something called contact inhibition). Cancer cells ignore these cells and invade nearby tissues.
Benign (noncancerous) tumors have a fibrous capsule. They may push up against nearby tissues but they do not invade/intermingle with other tissues.
Cancer cells, in contrast, don’t respect boundaries and invade tissues. This results in the fingerlike projections that are often noted on radiologic scans of cancerous tumors. The word cancer, in fact, comes from the Latin word for crab used to describe the crablike invasion of cancers into nearby tissues.
Related:What Is Invasive Ductal Carcinoma?
Energy Source
Normal cells get most of their energy (in the form of a molecule called ATP) through a process called the Krebs cycle, and only a small amount of their energy through a different process called glycolysis.
Many types of cancer cells produce their energy through glycolysis despite the presence of oxygen (Warburg phenomenon). Thus, the reasoning behind hyperbaric oxygen therapy is flawed. Sometimes hyperbaric oxygen may induce cancer growth.
Mortality/Immortality
Normal cells are mortal, that is, they have a lifespan. Cells aren’t designed to live forever, and just like the humans they are present in, cells grow old. Researchers are beginning to look at something called telomeres, structures that hold DNA together at the end of the chromosomes, for their role in cancer.
One of the limitations to growth in normal cells is the length of the telomeres. Every time a cell divides, the telomeres get shorter. When the telomeres become too short, a cell can no longer divide and the cell dies.
Cancer cells have figured out a way to renew telomeres so that they can continue to divide. An enzyme called telomerase works to lengthen the telomeres so that the cell can divide indefinitely—essentially becoming immortal.
Ability to "Hide"
Many people wonder why cancer can recur years, and sometimes decades after it appears to be gone (especially with tumors such as estrogen receptor-positive breast cancers). There are several theories about why cancers may recur.
In general, it's thought that there is a hierarchy of cancer cells, with some cells (cancer stem cells) having the ability to resist treatment and lie dormant. This is an active area of research, and extremely important.
Related:Why Does Cancer Come Back?
Genomic Instability
Normal cells have normal DNA and a normal number of chromosomes. Cancer cells often have an abnormal number of chromosomes and the DNA becomes increasingly abnormal as it develops a multitude of mutations.
Some of these are driver mutations, meaning they drive the transformation of the cell to be cancerous. Many of the mutations are passenger mutations, meaning they don’t have a direct function for the cancer cell.
For some cancers, determining which driver mutations are present (through genetic testing) allows providers to use targeted medications that specifically target cancer growth.
The development of targeted therapies such as EGFR inhibitors for cancers with EGFR mutations is one of the more rapidly growing and progressing areas of cancer treatment.
Related:Malignant and Benign Tumors: Key Differences
Can Cancer Cells Differ From Other Cancer Cells?
Given the many differences between cancer cells and normal cells, you might be wondering if there are differences between cancer cells themselves. That there may be a hierarchy of cancer cells—some having different functions than others—is the basis of discussions looking at cancer stem cells as discussed above.
Scientists still don't understand how cancer cells can seemingly hide for years or decades and then reappear. It's thought by some that the "generals" in the hierarchy of cancer cells referred to as cancer stem cells may be more resistant to treatments and have the ability to lie dormant when other soldier cancer cells are eliminated by treatments such as chemotherapy.
We currently treat all the cancer cells in a tumor as being identical, but it's likely that in the future, treatments will take some of the differences in cancer cells in an individual tumor into account.
Related:How Cancer Stem Cells Work
Summary
Some of the differences between normal cells and cancer cells are well known, whereas others have only been recently discovered and are less well understood.
Many people become frustrated, wondering why we haven't yet found a way to stop all cancers in their tracks. Understanding the many changes a cell undergoes in the process of becoming a cancer cell can help explain some of the complexity. There is not one step, but rather many, that are currently being addressed in different ways.
For researchers, understanding how cancer cells function differently from normal cells lays the foundation for developing treatments designed to rid the body of cancer cells without damaging normal cells.
In addition, cancer isn't a single disease, but rather hundreds of different diseases. And even two cancers that are the same with regard to type and stage, can behave very differently. If there were 200 people with the same type and stage of cancer in a room, they would have 200 different cancers from a molecular standpoint.
Related:How Many Types of Cancer Are There?
A Word From Verywell
As more is learned about what makes a cancer cell a cancer cell, more insight into how to stop that cell from reproducing—and perhaps even making the transition to becoming a cancer cell in the first place—is gained.
Progress is already being made in that arena, as targeted therapies are being developed which discriminate between cancer cells and normal cells in their mechanism.
Research on immunotherapy is just as exciting, as experts are finding ways to "stimulate" the immune system to do what it already know how to do—find and eliminate invaders.
Figuring out the ways in which cancer cells "disguise" themselves and hide has resulted in better treatments, and uncommonly, complete remissions, for some people with the most advanced solid tumors.
Related:Coping With a Cancer Diagnosis

