Brian Mazza Is Running 50 Miles to Fight Male Infertility Stigma

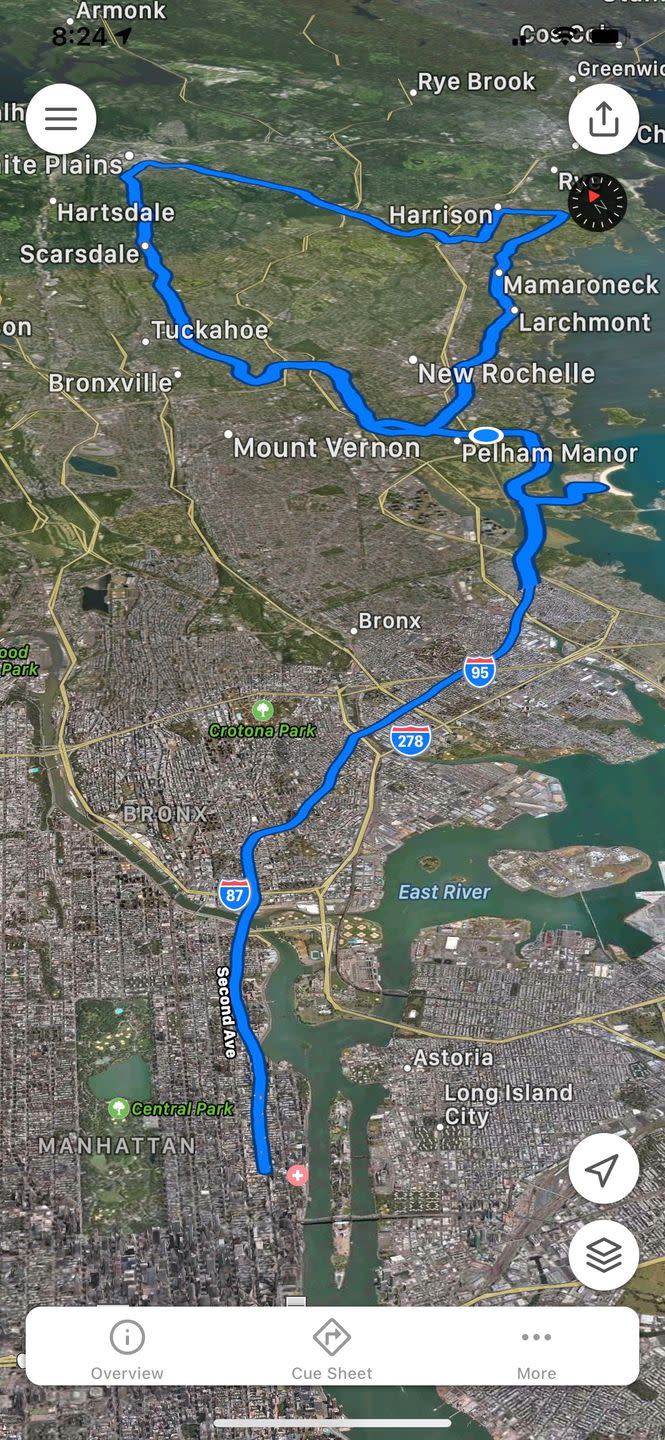
On December 12th, Brian Mazza will be running a grueling 50 miles, beginning in Manhattan and then trekking north up through the Bronx and into the hills of Westchester. Given the length and terrain, the ordeal will feel to Mazza like a double marathon. When asked if he’d ever done anything that long distance before, Mazza just laughs and then says quietly, “I have not.”
The goal is to raise money for infertility treatments for couples—many of whom, Mazza says, have had to delay family plans due to COVID-19, since treatment clinics have closed. By running, Mazza also hopes to destigmatize male-factor infertility—when the cause of a couple’s pregnancy complication is the male’s sperm. It’s an ignominy Mazza has been trying to dissipate since his own discovery four years ago. It was a moment that made him question is own manhood.
Before then, and for almost a year, Mazza and his wife, CNN journalist Chloe Melas, had been unsuccessfully trying for children. When Melas’s doctor recommended Mazza also get tested for potential fertility issues, he balked. Mazza works in business. He co-founded a chain of restaurant bars in 2009 and has since worked on other entrepreneurial projects across health and fitness. He’s twice appeared on the cover of Men’s Health Mexico. “I was like, ‘Why would I have to go get checked out?,’” he remembers thinking at the time. “‘I'm in great shape. I’m crushing business. Life is awesome. I don't need to get check out. It's not me.’”
An estimated 15 percent of all couples worldwide are infertile, meaning they are unable to conceive a child after one or more years of unprotected sex. The CDC estimates that in 35 percent of infertile couples, male infertility is an identifiable cause, though other calculations of the proportion of male-factor infertility are as high as 70 percent. Regardless of the exact percentage, the upshot is clear: infertility, which is far from an uncommon issue facing couples, is also, in many circumstances, a male issue.
While Melas’s own tests revealed she had low ovarian reserves (low number of eggs), Mazza soon learned he was also contributing to the couple’s infertility: his sperm count, it turned out, was also low.
What causes male-factor infertility?
There are several known factors that cause infertility in men, including structural formations during puberty, medical conditions such as diabetes and cystic fibrosis, as well as unhealthy habits—smoking, drinking, and steroid and illicit drug use. Male infertility can also be caused by various genetic or hormonal disorders. All of these factors can affect sperm health, number, and motility.

Mazza was right to think his fitness should help his fertility. Obesity has been shown to increase one’s risk of infertility; in one study, a man’s infertility odds were found to increase 10 percent for every 20 pounds he was overweight. But even though Mazza was beyond healthy, his habits weren’t the problem; some of us just have a low sperm count—regardless of how we eat or lift.
And a low sperm count makes conception that much more difficult. “Sperm have to be able to swim through the cervix up through the uterus into the fallopian tube, and then bind with the egg and cause fertilization to happen,” explains David Reichman, M.D., a reproductive endocrinology and infertility expert at Weill Cornell Medicine, as well as Mazza and Melas's doctor. “Sometimes the sperm cannot swim well enough to actually reach the egg. And other times it doesn't have the capacity to bind with the egg or fertilize the egg.”
To work around these difficulties, doctors can bypass the cervix and put the sperm directly into the uterus in what’s called “intrauterine insemination.” Should that process fail, there’s a more definitive procedure: in vitro fertilization (IVF), where eggs are retrieved from the female patient and then fertilized with the sperm outside the body in a lab. Dr. Reichman was fairly confident the procedure would work for Mazza, because Melas is young (and age, Dr. Reichman says, is the largest factor for fertility in women).

Why IVF treatment can be tough for men to accept
But doing a pregnancy this way can feel emasculating. “I really pride myself on being an alpha male in a positive way,” Mezza explains. “Not being able to do this—yeah, I didn't feel like a man. I wanted to be a father. And my body wasn’t allowing that to happen.” As a result, Mezza was embarrassed to reach out to friends or family with his situation.
“There’s more of a social fabric for women,” Dr. Reichman explains. “Women can get an AMH test to check their ovarian reserve. That’s often a springboard into meeting with a fertility specialist and talking about fertility goals—deciding whether to freeze eggs or when to pursue a family. For men, that fabric hasn’t historically existed.” The consequence: men don’t talk about infertility.
Mezza and Melas kept trying naturally to conceive. Mezza admits now his attitude was stubborn. After speaking to his doctor and researching the issue on his own, however, Mezza learned just how common male-factor infertility actually is. The reality of the situation became clear. “I always hoped that maybe we were able to [do it naturally],” Mezza says, “but I just saw the pain that it was creating within my wife. I knew that [IVF] was the next step for us.”

The treatment itself was not without stress and anxiety, but for the couple, it turned out to be a success, and Melas soon became pregnant with a boy. In 2017, Leo was born. Then, after another IVF treatment, Mazza and Melas welcomed another son, Luke. The couple call the boys their “miracle babies.”
Now, Mezza better understands his reaction—and how he may be able to use his story to get more men talking. “I was embarrassed as a man,” he admits. “Straight up. And that's just the god honest truth. But every time I look at my son, I don’t care what we had to do to get him. I really don't. So let’s talk about it. Let's help people if we can help people.”
Since in-person marathons were canceled this year due to COVID-19, Mezza wanted to launch a different endurance test, one that would be symbolic to the issue of male infertility. He decided to run 50 miles to raise money for others' treatment. (Fifty representing the statistic he read before embarking on IVF—that potentially over half of infertility cases are male-factor.) Mezza will begin at Weill Cornell Medical Center in Manhattan, where the couple did their IVF treatment, and end at his house outside the city, pushing a stroller with Leo and Luke for the final half mile.
As IVF treatment can often be expensive—with insurance not always covering the full procedure—Mezza is hoping to raise enough donations to help multiple couples grow their families. He’s also hoping that by seeing him run, other men might feel more confident sharing their own fertility issues with friends and family.
“More men need to speak about it,” says Mezza. “You're not inferior. You're not less of a man. You're fine. It's just a hiccup.”
To make a donation to help families with fertility treatment, visit Weill Cornell Medicine.
You Might Also Like

