Breast cancer screening: Everything you need to know
In 2018, breast cancer is still the most common cancer in the UK. According to the National Health Service, around one in eight women are diagnosed with the disease during their lifetime.
It also has, arguably, one of the highest profiles of any form of cancer - campaigning around the disease has been prolific, particularly in the past 20 years, with more and more women in the public eye speaking out about their own experiences.
Every woman knows someone who has had it, most know someone who has died from it. We all know - we think - how to protect ourselves.
We check ourselves in the shower, we talk about our breasts with our friends, mothers and sisters. And we know that after a certain age we'll need to get regular mammograms.
But even though breast cancer is still the most common cancer in this country, the mortality rates are falling. Why? Because the number of women diagnosed every year is rising.
New treatments and clinical trials and - crucially - early diagnosis have all been key to reducing the number of lives claimed by the disease.
It's why the news that up to 270 women may have died as a result of a major NHS computer error which meant 450,000 were denied breast cancer screening, is so concerning.
The NHS currently screens all women between the ages of 50 and 70 for breast cancer every three years. Women over 50 should receive a letter from their GP about the test which aims to catch cancer early, when it is easier to treat, and when it hopefully hasn't spread anywhere else in the body.
But Jeremy Hunt, the Health Secretary, announced today that around 450,000 women aged 68 and over did not receive an invitation for screening.
Since then around 150,000 have died - many from other illnesses - with 270 likely to have had their lives cut short as a result of the blunders.
With the help of Breast Cancer Care, we look at why screening is essential to breast cancer diagnosis, what it entails, and how to get it.
Why is breast screening offered?
A review of the NHS Breast Screening Programme in 2012 concluded that in a year, screening prevented 1,300 deaths from breast cancer.
Going for a screening can help find cancer before it can be physically felt or seen. Many women know how to check themselves for signs of cancer, but it can't always be detected by feeling a lump. A screening could detect a tumour too far back in the chest to be obvious externally, and could detect cancerous cells which haven't even turned into a tumour yet.
Prostate and Breast cancer deaths in UK
Breast Cancer Care say: "Invasive breast cancers (which can spread to other parts of the body) found through screening are more likely to be found earlier and respond very well to treatment.
"This means a mastectomy (removal of all the breast tissue including the nipple area) and chemotherapy is not always needed."
When will I be offered breast screening?
To be invited for screening, you have to be registered with a GP. The screening service takes the names from your GP’s list at regular set times and you’ll be sent an appointment to come for a mammogram.
This may not happen the year you turn 50, but it will happen by the time you are 53.
Jeremy Hunt's announcement revealed that the women who were missed due to a computer glitch were between the ages of 68 and 71 (the cut-off for women to be sent invitations for screening is 70).
Women under 50 are not invited for routine breast screening, because the number of women who get breast cancer is much lower in this age group.

Eighty one per cent of breast cancers occur in women over the age of 50, and the risk continues to increase with age.
The breast tissue in younger women can be dense, which can make the X-ray image less clear. This makes normal changes, benign breast conditions and cancer harder to find.
If you’re over 70, you won’t be sent an invitation for screening. However, you can continue to have breast screening every three years if you ask for it. Your GP’s surgery can put you in touch with your local breast screening unit or you can look them up online.
Find out about screening in Scotland, Wales, England and Northern Ireland here.
What happens at a routine breast screening appointment?
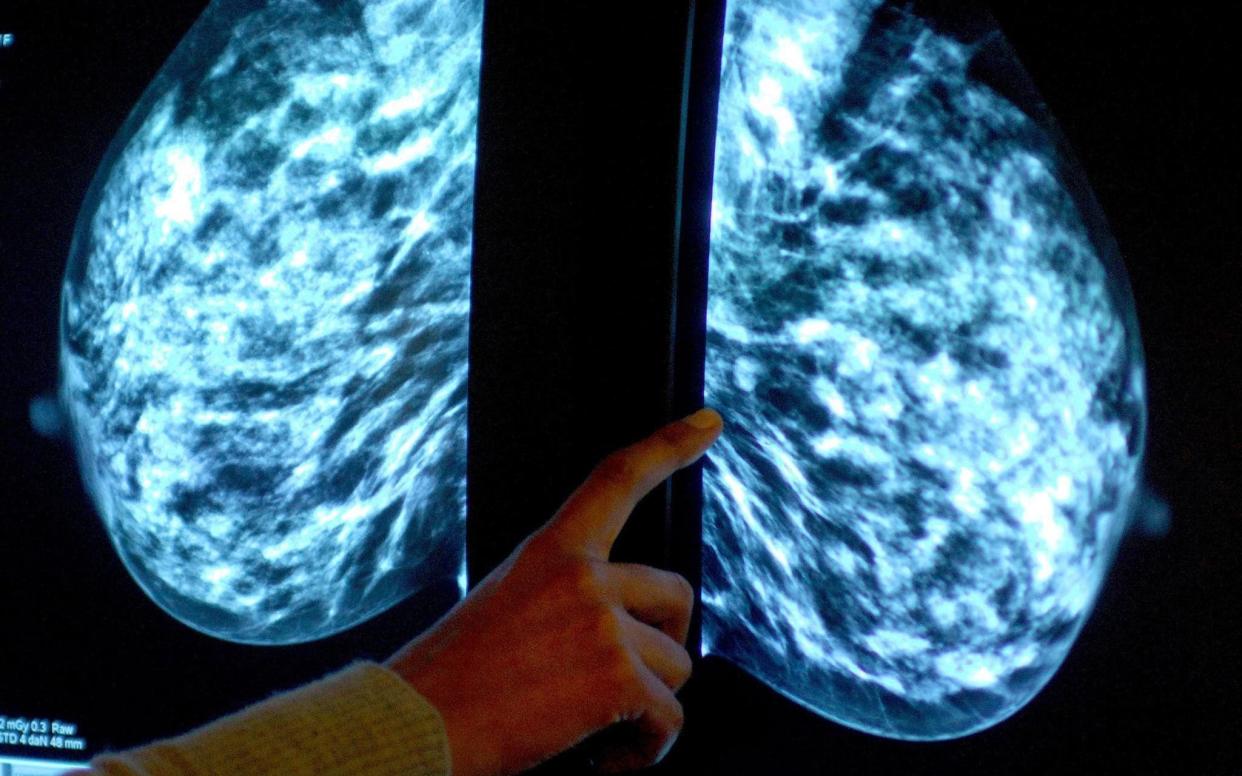
Mammograms
Your mammogram will usually take place at a breast screening unit, but in some areas you'll be invited to a mobile unit.
A female practitioner will take your mammogram, which is essentially a breast X-ray. You will be asked to undress to the waist and stand in front of the machine. Your breasts will be placed one at a time on the x-ray machine. The breast will be pressed down firmly on the surface by a clear plate.
At least two pictures of each breast will be taken, one from top to bottom and then a second from side to side to also include the part of your breast that extends into your armpit.
You will need to stay in this position while the x-ray is taken. You may find it uncomfortable, but it only takes a few seconds and the compression doesn’t harm the breasts.
Further mammograms taken at different angles or with magnification are sometimes used to examine particular areas of the breast in greater detail.
Digital breast tomosynthesis (DBT)
This is another type of mammogram that is being trialled in some hospitals. DBT makes 3D pictures using X-rays. The breast is positioned the same way as when having a mammogram, but less pressure is applied – just enough to keep the breast in a stable position. The X-ray arm rotates and curves around the breast, taking multiple X-ray pictures at different angles. The information is then sent to a computer where it turns the pictures into three-dimensionalised images (3D mammogram).
Ultrasound scans
An ultrasound scan will usually be done in addition to mammograms, regardless of your age. They are often used together because they provide different information.
It uses high-frequency sound waves to produce an image of the breast tissue.
You’ll be asked to undress to the waist and lie on a couch with your arm above your head. To help gain a clear image of the breast, some gel will be spread over the area of your breast being scanned. The doctor or nurse will use a hand-held scanning probe, which will be moved over the breast to look at the underlying breast tissue. The area under your arm (axilla) may also be scanned.
Why family history matters
Having someone in your family with breast cancer doesn’t always mean your own risk is increased.
However, a small number of women have an increased risk of breast cancer because of their significant family history and may be offered breast screening earlier and more frequently.
If you have been assessed as being moderate or high risk of breast cancer, you will be offered regular scans and/or mammograms to check for breast cancer.
According to Breast Cancer Care, "If you’re at high risk, the type of screening will also depend on your individual likelihood of being a gene carrier. If you are told that you have more than a 30 per cent chance of being a gene carrier, your screening will start earlier and go on for longer."
• For more details, go to nhs.uk/conditions/breast-cancer

