What Is Allergic Asthma?
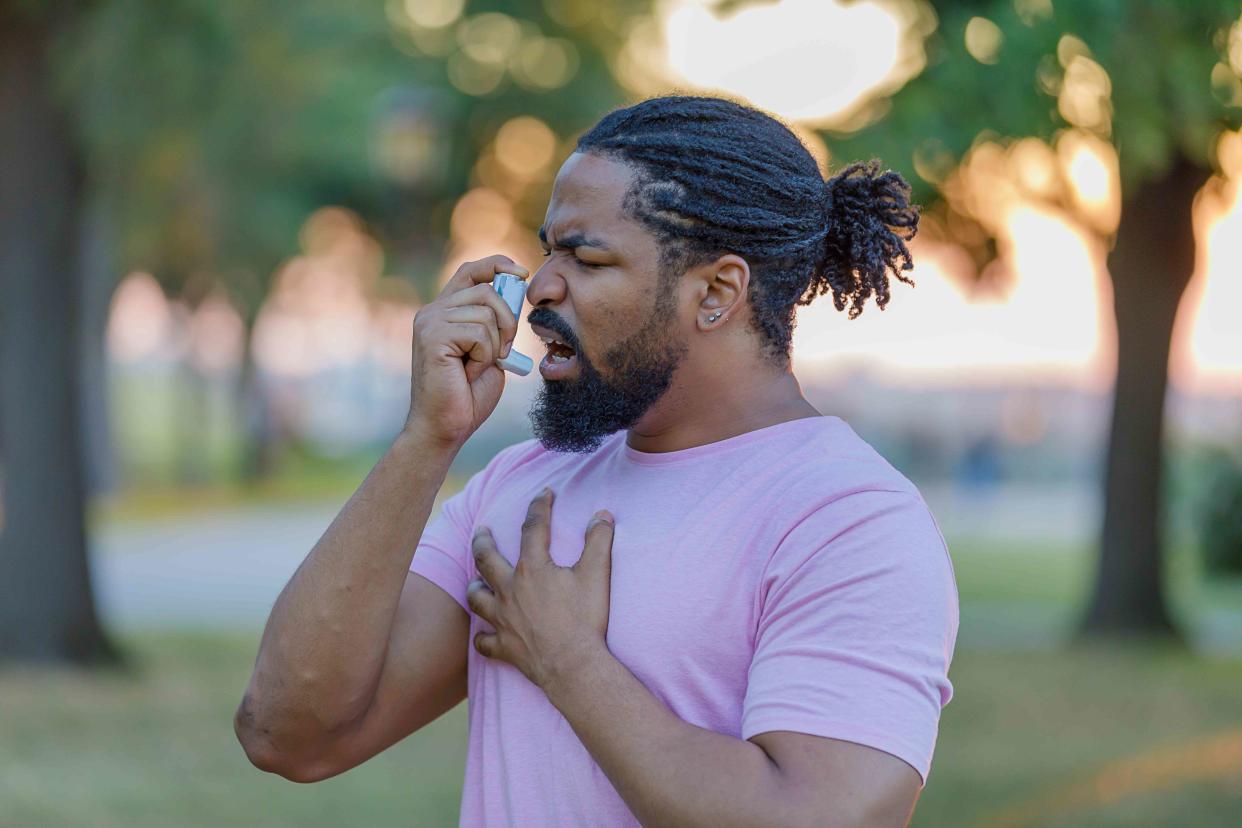
ProfessionalStudioImages / Getty Images
Medically reviewed by Daniel More, MD
Allergic asthma is a chronic (long-term) breathing condition in which your airways become inflamed and narrow in response to inhaling allergens like pet dander, dust mites, and pollen. With allergic asthma, exposure to allergens triggers an overactive immune response, leading to symptoms of an "asthma attack" like coughing, wheezing, chest tightness, and dyspnea (shortness of breath).
Allergic asthma is the most common form of asthma, accounting for about 80% of childhood asthma and 50% of adult asthma cases. It's caused by a combination of genetic and environmental factors. Treatment helps manage symptoms, and lifestyle modifications can reduce the frequency of asthma attacks.
Allergic Asthma Symptoms
Allergic asthma symptoms can vary from person to person, ranging from mild to severe. Most people with allergic asthma experience respiratory (breathing-related) symptoms similar to symptoms of other asthma types. They also experience allergy symptoms.
Respiratory Symptoms
Inhaling an allergen causes your airways to become inflamed and swollen. This can cause respiratory symptoms such as:
Wheezing: Whistling sounds when you breathe
Coughing: A dry cough (without mucus)
Shortness of breath: Feeling like you can't take a deep breath or get enough air in your lungs
Chest tightness: An uncomfortable sensation of chest pressure, tightness, or discomfort
Allergy Symptoms
People with allergic asthma also typically develop allergy symptoms after exposure to an allergen. These symptoms include:
Runny or stuffy nose with clear mucus
Sneezing
Red, watery eyes
Itchiness around the eyes, mouth, or nose
What Causes Allergic Asthma?
With allergic asthma, your airways become overly sensitive to specific inhaled allergens like dust mites, pollen, or pet dander. These substances are usually harmless, but if you have allergic asthma, your body sees them as a threat and triggers an overactive immune response.
Your immune system produces immunoglobulin E (IgE) antibodies to fight off the perceived threat, which causes your body to release chemicals like histamine, cytokines, and prostaglandins. These chemicals inflame your airways and lead to asthma symptoms like shortness of breath and wheezing.
Genetic and environmental factors play a role in the development of allergic asthma.
Genetics
Researchers have identified over 100 genes associated with an increased risk of developing allergic asthma. These genes influence various aspects of your immune system and lung function, including:
Overactive immune response: Certain genes control your immune system's response to allergens. For example, interleukin-4 (IL-4) and interleukin-13 (IL-13) are substances called cytokines that play a role in airway inflammation. Variations in genes responsible for producing these cytokines can make you more susceptible to airway inflammation when you come into contact with allergens.
Epithelial barrier dysfunction: The epithelial barrier in your airways protects your body from environmental threats like allergens and infectious microbes (e.g., bacteria). Mutations (variations) in genes that regulate how epithelial cells function can disrupt how the barrier functions. This makes it easier for allergens to enter your airways and cause inflammation.
Smooth muscle function: Variations in genes that help smooth muscle function in your airways can contribute to airway hyperresponsiveness. This means that your smooth muscles contract more quickly in response to environmental triggers, which causes your airways to narrow.
Environmental Triggers
People with allergic asthma may develop symptoms in response to indoor or outdoor allergens. Common triggers for allergic asthma attacks or episodes include:
Pollen from trees, grasses, and weeds
Pet dander
Mold
Dust mites
Cockroaches (feces, body parts, saliva)
Risk Factors
Allergic asthma can affect people of all ages. Certain factors can increase your risk, including:
Family history: Having a family member with allergies or asthma increases your risk of allergic asthma.
Early life exposures: Exposure to allergens and irritants in early childhood, such as secondhand smoke or dust mites, is associated with an increased risk of allergic asthma.
Other allergic conditions: People with other allergic conditions are more likely to develop allergic asthma. This includes eczema (a group of chronic skin conditions that can cause inflammation, irritation, and swelling of your skin) and allergic rhinitis (seasonal allergies).
Socioeconomic factors: Lower socioeconomic status is associated with a higher risk of allergic asthma. Factors like living in a more rural area, increased exposure to allergens and airway irritants, and limited access to healthcare may play a role.
How Is Allergic Asthma Diagnosed?
Diagnosing allergic asthma involves a thorough medical history review and physical exam by a healthcare provider, such as your primary care provider or an allergist. An allergist is a doctor who specializes in diagnosing and treating allergies, asthma, and other conditions related to your immune system.
Your healthcare provider will ask about your symptoms, including how often they occur, how severe they are, and what triggers them. They will examine your eyes, ears, nose, throat, and skin and listen to your lungs for signs of asthma-like wheezing.
Diagnostic tests can help confirm an allergic asthma diagnosis by ruling out other possible causes of your symptoms. They include:
Spirometry: This is a lung function test that involves breathing into a mouthpiece connected to a machine (spirometer) to measure how much and how quickly you can forcibly exhale air from your lungs.
Indirect bronchoprovocation: Your healthcare provider exposes you to specific allergic asthma triggers (e.g., pollen) and observes how your airways react. This helps determine which allergens trigger symptoms. This form of bronchoprovocation isn't performed outside of research institutions.
Direct bronchoprovocation: You inhale a specific concentration of a substance like methacholine, which causes bronchospasm (airway tightening). At a certain concentration of methacholine, this can be diagnostic of asthma.
Fractional exhaled nitric oxide (FeNO) test: This measures the amount of nitric oxide in your breath when you breathe into a handheld device. It measures airway inflammation. The FeNO test is more often used to diagnose eosinophilic asthma—asthma caused by overactive white blood cells in your lungs.
Skin prick test: Your healthcare provider scratches a tiny amount of a possible allergen into the surface of your skin to see if an allergic reaction (e.g., redness, swelling, bumps) develops in response to the substance.
Blood tests: Immunoglobulin E (IgE) is a common blood test. IgE is an antibody produced by your immune system in response to an allergen. People with allergic asthma typically have a high level of IgE in their bloodstream.
Treatments for Allergic Asthma
There is no cure for allergic asthma, but treatments can help manage symptoms. They can also keep your airways open to prevent future symptom flares (asthma attacks). Your healthcare provider will work with you to develop a personalized treatment plan, sometimes called an asthma action plan.
Medications
Many medications reduce allergic asthma symptoms. Your healthcare provider may prescribe:
Quick-relief medications: Bronchodilator medications, such as short-acting inhaled beta2-agonists and anticholinergics, work quickly to relieve allergic asthma symptoms when they develop. These drugs relax and open your airways to make breathing easier. You breathe them in through an inhaler or nebulizer to quickly relieve symptoms when they develop.
Controller medicines: Daily medications can reduce inflammation and keep your airways open. Your healthcare provider may prescribe inhaled corticosteroids such as Flovent (fluticasone) or Pulmicort Flexhaler (budesonide). Oral anti-leukotriene medicines taken by mouth, such as Singulair (montelukast sodium), can block the action of immune chemicals that cause inflammation.
Biologics: Biologics are therapies that contain a living substance. Some biologics target specific cells, proteins, and pathways that inflame airways. For example, Xolair (omalizumab) blocks IgE antibodies that cause airway inflammation in people with allergic asthma.
Antihistamines: Antihistamines block histamine—the chemical that causes allergy symptoms like runny nose, itchiness, and watery eyes. They're available over-the-counter (OTC) and by prescription. Your healthcare provider may recommend using an antihistamine like Claritin (loratadine), Allegra (fexofenadine), or Zyrtec (cetirizine) when needed. They may recommend taking it daily to prevent allergy symptoms when your allergies are most severe (e.g., seasons with higher pollen levels).
What is a nebulizer?
A nebulizer is a device that turns liquid medicine into mist or aerosol that you inhale directly into your lungs. Unlike inhalers, nebulizers don't require a specific breathing technique: you simply breathe normally into the mouthpiece or mask. Because of this, they can be easier to use than inhalers for some people, including young children and people with severe respiratory conditions.
Immunotherapy
Allergen immunotherapy helps build your tolerance to allergens. It reduces or eliminates your symptoms. Immunotherapy decreases your sensitivity and response to allergens like pollen, animal dander, dust mites, cockroaches, and mold over time.
Most allergen immunotherapy treatments involve getting injections, or allergy shots, regularly—for example, once a week to once a month. A course of immunotherapy is for 3-5 years total. The buildup phase typically lasts 3-6 months (weekly shots), until the target dose is reached. You'll then enter the maintenance phase, which is shots every 2-4 weeks for a total of 3-5 years.
How To Prevent Allergic Asthma
There is no guaranteed way to prevent allergic asthma, but you can reduce the risk of attacks. Your healthcare provider will discuss these strategies with you as part of your asthma action plan:
Identify and avoid triggers: This is one of the most effective ways to prevent allergic asthma attacks. It may involve using allergy-proof bedding to reduce dust mite exposure, installing air purifiers in your home, or checking local pollen forecasts and staying indoors during peak pollen times.
Follow your treatment plan: Take your medications as prescribed, even when you are symptom-free, to help control inflammation and keep your airways open.
Use a peak flow monitor: Blowing into a small device called a peak flow monitor can help detect narrowing in your airways, sometimes before symptoms develop. It works similarly to how a thermometer measures body temperature. Your healthcare provider will tell you what your readings mean to help identify when to take quick-relief medicine, how much to take, and when you should call your healthcare provider or go to an emergency room visit for immediate medical care.
Related Conditions
Having allergic asthma may increase your risk of developing various conditions. These include:
Atopic dermatitis (eczema): This is a chronic inflammatory skin condition that causes itchy, inflamed skin. It often develops before allergic asthma. The two conditions share many links, including allergen sensitivity, immune system dysfunction, raised IgE levels, and genetic factors.
Sinusitis: Allergic asthma can cause acute (short-term) or chronic sinusitis. Sinusitis is inflammation of your sinuses—air-filled cavities near your nose, eyes, cheeks, and forehead. It leads to mucus build-up in your nasal passages and makes asthma symptoms worse.
Gastroesophageal reflux disease (GERD): GERD is a condition in which stomach acid backs up into your esophagus (a muscular tube that helps move food and liquid from your throat to your stomach). It causes symptoms like heartburn. Asthma can trigger the development of GERD and vice versa. GERD can also worsen asthma symptoms such as cough and breathing difficulty.
Obesity: Obesity is associated with chronic inflammation, which research suggests may cause airway inflammation and contribute to asthma. Excess body fat can reduce also the effectiveness of certain allergic asthma medications (e.g., corticosteroids) and increase the risk of severe symptoms.
Living With Allergic Asthma
Living with allergic asthma can be a frustrating and sometimes frightening experience. It's a chronic condition that requires ongoing management, but it doesn't have to limit your quality of life. It's a controllable condition if you have an effective treatment plan.
Well-controlled asthma allows you to engage in daily activities, sleep through the night, and exercise without symptoms or requiring quick-acting medication. In short, you can live an active and fulfilling life by working closely with your healthcare provider, actively managing your triggers and symptoms, and following your treatment plan.
Talk to your healthcare provider if you think that your treatment plan isn't working as well as you'd like or if you notice a change in your symptoms.
Frequently Asked Questions
How serious is allergic asthma?
Allergic asthma can be serious, but most people with allergic asthma can live full and active lives with proper treatment and management. Uncontrolled asthma can lead to frequent flare-ups (asthma attacks) and limit daily activities. It can also be life-threatening if untreated. Avoiding triggers, following your treatment plan, and knowing when to seek emergency care are essential for allergic asthma management.
Is allergic asthma curable?
Allergic asthma is not curable, but it's manageable with proper treatment. This may involve medications, avoiding allergens that trigger symptoms, and consistent symptom monitoring.
How long does it take for your lungs to recover from allergies?
The time it takes for your lungs to recover from inhaling allergens can vary depending on the severity of symptoms and your overall health. Most people's lungs recover within 1-2 weeks after a severe allergic asthma attack.
For more Health.com news, make sure to sign up for our newsletter!
Read the original article on Health.com.
