An Air Force Nurse Deployed to NYC Hospitals: 'It Feels Like a Warzone'

In April, as New York City emerged as the epicenter of the Covid-19 pandemic, the U.S. military deployed 720 troops to work in the city’s overburdened medical centers. One such service member is 36-year-old Rosa Blackdeer, a registered nurse and First Lieutenant in the Air Force Reserves, who left her family behind in Wisconsin to serve at Lincoln Medical Center, a public hospital in the Bronx that is home to the busiest emergency department in NYC. Here is her story, told in her own words:
New York City was supposed to be the destination of our family summer vacation this year. I arrived on April 5. My unit is staying at a hotel in Times Square. I’ve never been here before, but from watching movies and TV shows, I know what it’s supposed to look like, and it is crazy to see everything empty. It’s like a Walking Dead episode.
My alarm goes off at 5 a.m. I heat up oatmeal in my microwave for breakfast. I got one for my room because otherwise there’s only one microwave for like 20 floors. Then, I make a sack lunch: a sandwich, an apple, and some grapes. I don’t want to eat or prep food anywhere else but here.
Then, I get my scrubs on and pack a bag with my nursing shoes, goggles, booties, head cover, and my N95, which I carry in a Tupperware container. We’re able to get four N95s per person at a time; we number them and rotate through them, letting them airdry to kill the virus between wears. I hang mine on little plastic hooks I stuck to the back of my hotel room door. I wear one surgical mask when I leave my room and take an extra; we wear them on top of our N95s all day. Sometimes the hospital has them, but right now we’re getting them from the military. We meet downstairs once a week and our supervisor hands us the masks we need for the week. I wish I had a whole box of them. We’ve also had our families and hospitals back home send us supplies. But otherwise we’ve been googling stuff to buy online, just like everybody else.
At 5:45 a.m. I meet my buddy, a woman from my unit named Kristy, and we walk to the Javits Center together to catch a bus to the hospital. It’s dark and cold walking there and you never know what you’re going to find. One day there was a big pile of human feces on the sidewalk and I was like, Oh, that’s great. Welcome to New York.
My husband was in the military for eight years, so he knows what it feels like when orders come down. I told him I had to leave in the morning and at first he was like, “What?!” But then he said, “Okay.” My husband works at a gym as a personal trainer, but he got laid off because of Covid; we have two kids, ages 13 and 14, and a foster child, a five-year-old that we just got in August. When I deployed in the past, my kids were babies and didn’t know. They just thought, Mommy has gone away. But now, it’s a very different experience because they’re like, “Wait. Hold on. You’re going to Ground Zero?” So, it’s harder on them, but I think the kids were mostly concerned that “Dad only makes us pizza.” But I told them they’d be fine, and I’m very proud of my husband—he’s doing pretty good.
When we board the bus, everyone is like, “Ready to do this?” and we’re like, “Yeah, here we go again.” We take two buses so everyone gets their own seat, for safety. Before I get off the bus, I put my N95 on because sometimes there are patients or homeless people waiting near the hospital entrance. I don’t like to put my N95 on any sooner than I have to, though, because my nose is pretty messed up from it—irritated, red, and sore. Sometimes I want to put a Band-Aid on it, but I’m also scared. Is it going to mess up the seal?
We get to Lincoln around 6:40 a.m. The hospital looks so dreary when we’re walking in. After I’m inside, the first hand sanitizer dispenser I get to is empty.
I am working on a floor that was created maybe two days before I got here. It’s the third new unit the hospital has created to treat Covid-19 patients. We’re trying to do our best, but the floor used to be a clinic and really wasn’t created for in-patient care, so we’re running back and forth constantly trying to find everything we need. I am typically assigned to four patients and there are about 25 in total, which is a lot of patients for a unit that shouldn’t really exist.
Ninety-five percent of my patients have tested positive for Covid-19. There are about 35 people from my unit that got sent to Lincoln and no one has come down with symptoms yet, so that’s good. But it’s hard too because we’re putting ourselves on the front line and the enemy is invisible. In war, you can tell who the enemy is—here, you can’t see it. It’s like, did I touch something wrong? Did I put mask on differently? The anxiety that comes with that is hard. Once, someone coughed in my face and I thought I felt it go through my goggles. The mental drainage is intense, like, Oh my god, I hope I didn’t just get it.We’re all scared. We see who this virus is affecting—young or old, it doesn’t matter. I come to work every day and I don’t know if that’s the day I’m going to get it or not.
I eat my lunch in the breakroom, but it just doesn’t look clean. The table is sticky so I always bring my own Clorox wipes to wipe everything down before I eat. I don’t feel like it’s really a break because I have to pay attention, like, oh my god, did I touch something?
I was stationed in Balad, Iraq in 2009 for six months. Back then, I was a med tech and we did a lot of patient transfers to hospitals in Germany and elsewhere. We had busy days—sometimes we moved like 50 patients a night, busting our butts, carrying 200-plus pound guys—but it’s definitely a different busy here because our patients decline so quickly. One minute they’re breathing well and then all of a sudden it’s like, Oh my god, what just happened? Supply-wise, it’s the same. We always have issues with supplies, so I’m used to being creative. We call it MacGyver nursing.
The work hits me harder here because it’s right on our own soil. At least when I’m in a war, I know everyone there signed on the dotted line saying they are going to fight for our country. You’re expecting mass casualties and bodies to be coming in because that’s the environment you’re in. You don’t expect that when you’re stateside. I’m treating civilians who could be my family. In fact, most nurses on my floor are from New York, so this is their home and they are losing family members. Nurses have died who were working at Lincoln. It definitely feels like I’m in a warzone sometimes.
One that hit me hard was a 94-year-old woman. We knew she wasn’t going to make it. Some people say it’s easier when it’s an older person, but it’s still hard, especially now when they don’t have family with them. We were trying to talk to her every chance we got. I would talk to her about the weather and hold her hand if I had time. When she started to go, I had to run and get the doctor to see if there was anything else we should do. I had to leave, but I didn’t want her to die by herself. So as I was running out the door, I said to a colleague, “Please, just go in there and hold her hand.” Nobody should die by themselves.

I’m a manager at the hospital where I work in Wisconsin. Before I left home, 11 people had tested positive for Covid-19 in our little small town of about 3,000 people. I told everybody, “Hey, we’re going to make it through. The need is greater somewhere else.”
The deaths really weighed on the members of my unit when we first got here. We’re not used to seeing so many. What we decided to do is, whenever we have a death, regardless of how busy we are, we all get together in that room and we say thank you to the team. “Thank you for doing your part. Regardless of what happened, we know you did your best to keep them alive.” We were there for these patients even when their families couldn’t be and it’s important to acknowledge that. We have a moment of silence, and then we move on with our days.
Sometimes you have patients who you don’t think are going to make it, and they do. One time I had a patient who was 68 or 69 years old with three or four comorbidities and I really didn’t think she was going to pull through. She had a high fever for two days and I had icepacks on her everywhere, but it was getting to the point where there was nothing I could do to make her more comfortable. I felt really defeated because usually there’s always something else you can do. Every time I would go into her room, it was horrible because she’d be like, “Just let me die. I can’t do this anymore.” I was like, "No, you can. We're going to try our best to make it through this." She's like, "No, just let me die." And I'm like, "Yes, we can. We're strong."
When I came back to work for my next shift a few days later, she was doing much better. Her fever was lower, she was talking more and even laughing. She wasn’t my patient anymore, but you get used to these patients when you have them for a while. Not to say they’re family, but you have a connection. So I was still checking on her. I asked her if she knew who I was because sometimes patients with high fevers don’t remember things. She was like, “Yeah, didn’t I tell you to let me die?” And I’m like, “Yeah, aren’t you glad I didn’t listen to you?” She’s like, “Oh yes,” chuckling. She said she couldn’t believe she made it through. She was eventually able to go home. I really didn’t know if she was going to be a success story or not, but she made it. I was like, you have got to be kidding me—I was so happy.
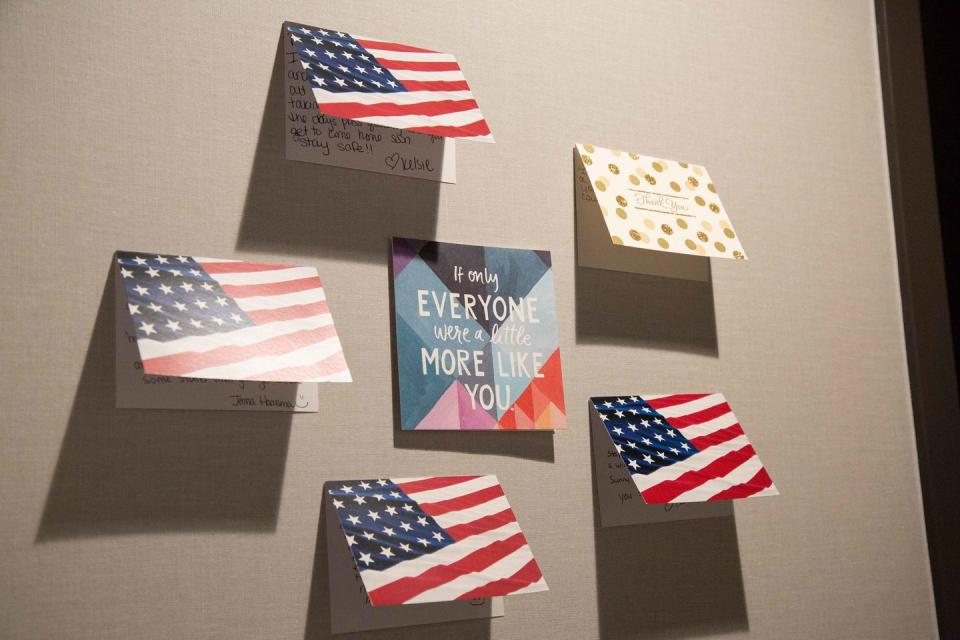
We got to see one of our patients get extubated the other day, which was a big deal because not too many patients who get intubated survive. He was only 37. It takes a while for all of the medication to wear off in the body. It was a rough few days, but he came back little by little. He even walked to the wheelchair by himself when it was finally time for him to be discharged. We got him a card and some balloons, and we got ourselves some little pompoms and lined up on either side of the hallway to cheer for him as he was wheeled out. We were so excited for him to go home. Anytime our patients are looking better from one day to another, we get so happy. You would think you’re giving us candy.
A lot of things that should be easy take longer here. The pharmacy is so overwhelmed that it can take over three hours to get medications. Some of my patients weren’t getting their morning meds until almost noon. It’s hard to work at a big hospital period, let alone at a big hospital with three new units of patients and the same number of pharmacists.
Another issue is we aren’t allowed to wear stethoscopes because of the risks of contamination. Every patient is supposed to have one in their rooms, but that is not always true and it’s really hard to do my job without one. I have to ask, “How do you think you’re breathing? Do you feel like it’s getting better?” I feel defeated because I don’t always have what I need to help someone. It’s hard not to take that feeling with you. Even when you’ve done everything possible, it sucks sometimes because you know you could have done better if you had the right supplies.
I hand off my patients around 6:40 p.m. and get ready to head back to my hotel. Once we’re on the bus, we’re all talking about what to order for dinner and texting with our colleagues back at the hotel. The members of our unit who have the day off are responsible for ordering for the group each day—that’s how we take care of each other.
When I get to my room, I take my shoes off and my other shoes out of my bag and spray both with Lysol and leave them in the hallway. Then I take a Clorox wipe to open and close the door. I take off my scrubs off—I have a laundry bag right by the door to put them in—and hang my N95 mask up to dry. Then, I go to the sink, wash my hands, and get in the shower.

By the time I’m clean, the pizza has arrived and my unit has set up a buffet in the hallway for family dinner. We Lysol the floor before we sit down and try not to touch anything. We’re like, eww, but sitting on the floor in the hall to have dinner together is still better than eating alone. We vent; we talk about the good and bad parts of our days. We know it’s not good to keep it all in, so it’s like our family therapy. We give only so much time to vent, and then we’re like “No more work talk!” And then we shift to our kids and spouses, or what we might do on a day off. One night we did sheet masks after dinner.
Sometimes, we’re speechless. We walked into the worst thing any of us have ever seen in the United States. Every day, you’re just going, going, going, and not seeing patients get better. The first weeks we were here, there wasn’t a day that when by that we didn’t have a death on the floor. One day we ran out of body bags. Another day there wasn’t anyone available to come pick up the deceased, so we had a dead body in a patient room next to a live patient for like six to eight hours. We’re just like, “This sucks!” There’s nothing else to say.
After I got my orders to go to New York back in April, I went to Walmart and bought what I thought I would need: Lysol spray, disinfecting wipes, etc. I also bought a pinata and some candy. When I got home, my kids helped me pack—I made a checklist so everyone could be involved. And then we went outside and hit the heck out of a pinata and celebrated everyone’s birthday, so I wouldn’t miss them.

In those first weeks, after work, I came into my room and cried in the shower. I cried again while talking to my husband. And then you just wake up the next morning and do it all again. I never thought in my whole career that I would see something like this. When I talk to my nurses back home and they ask how it’s going, I'm like, "I wouldn't wish this on my worst enemy." I hope I never have to deal with something like this again.
You Might Also Like

