Advanced Lung Cancer and Immunotherapy
Medically reviewed by Archana Sharma, DO, FAAP
Immunotherapy is a newer class of treatment for lung and other cancers. It primes the body’s natural immune system to fight back against cancer. Immunotherapy has been shown to improve survival in some types and stages of lung cancer.
Lung cancer immunotherapy was first approved by the Food and Drug Administration (FDA) in 2015. It has since become an essential new lung cancer treatment for early, recurrent, and advanced lung cancers.
This article will explain how immunotherapy works for different stages of lung cancer. It will discuss the impact of these therapies on life expectancy and survival rates. It will cover the benefits of immunotherapy, the potential side effects, the different types of immunotherapy, and the brand names used for specific classes and stages of lung cancer. It will also explore what the process of getting immunotherapy is like.
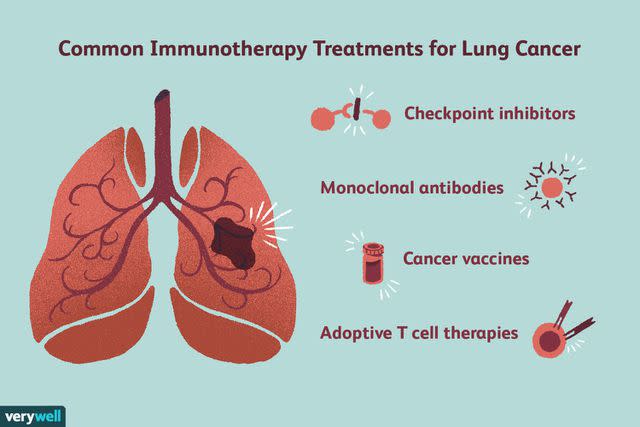
Verywell / Joules Garcia
Immunotherapy: An Emerging, New Lung Cancer Treatment
Immunotherapy drugs work by taking the brakes off the immune system or priming the immune system to fight cancer cells. A few therapies based on this approach are currently being used or tested against lung cancers. They include immune checkpoint inhibitors, cancer vaccines, and chimeric antigen receptor (CAR) T-cell therapy.
Related: Immunotherapy for Cancer: What Are My Options?
Checkpoint Inhibitors
The immune system has natural mechanisms to prevent it from damaging the body's healthy cells. Cancer cells sometimes take advantage of these mechanisms, called checkpoints, to hide from the immune system.
Immunotherapies called immune checkpoint inhibitors unlock these switches, letting the immune system “see” and attack the cancer.
Two main types of checkpoint inhibitors have been approved by the FDA for use against lung cancer. Those that target the programmed cell death protein 1 (PD-1)/programmed cell death ligand 1 (PD-L1) mechanism and those that target cytotoxic T-lymphocyte-associated protein 4 (CTLA-4).
Some immunotherapies target the PD-1/PD-L1 mechanism. When PD-1 on T cells (a type of immune system cell) binds to PD-L1 on the body’s cells, it keeps T-cells from attacking them. Drugs that block this binding boost the immune response against cancer, shrinking some tumors or slowing their growth.
Immunotherapies that block the CTLA-4 mechanism work similarly. CTLA-4 is another protein on T cells that keeps them from attacking healthy body cells. These immunotherapies are often used in conjunction with a PD-1/PD-L1 inhibitor.
CAR-T Cell Therapy
Chimeric antigen receptor T cell therapy, or CAR-T cell therapy, is a procedure to train the body’s T cells to fight cancer. These cells are removed from the body and changed in the lab. They’re given genes that help them find and fight cancer.
These changed cells are then infused back into the person with cancer, where they seek out and destroy cancer cells. Currently, CAR-T cell therapies are being tested in clinical trials for different types of lung cancer.
Cancer Vaccines
Cancer vaccines are treatments used to prime the immune system to find and fight cancers. They show the body cancer-related proteins and molecules. The immune system recognizes these proteins in the cancer cells in the body and hunts them down. Currently, cancer vaccines for lung cancer are being tested in clinical trials.
Types of Lung Cancer Immunotherapy
The three types of lung cancer treated with immunotherapy are:
Small cell lung cancer (SCLC) makes up 10% to 15% of lung cancers.
Non-small cell lung cancer (NSCLC) accounts for 85% to 90% of lung cancers. These include adenocarcinoma (40% of lung cancers), squamous cell (epidermoid) carcinoma (25% to 30% of lung cancers), and large cell (undifferentiated) carcinoma (10% to 15% of lung cancers).
Mesothelioma is a less common lung cancer that arises in the thin layer of tissue that covers the lungs.
Immunotherapy drugs are given as an intravenous (IV) infusion, typically through a port or peripherally inserted central catheter (PICC) line into a vein. You’ll need to get the infusion at a medical office, infusion clinic, or hospital.
Immunotherapies approved to treat lung cancers include:
Libtayo (cemiplimab) is injected over 30 minutes every three weeks.
Jemperli (dostarlimab) is injected over 30 minutes, once every three weeks for four cycles, and then once every six weeks.
Opdivo (nivolumab) is injected over 30 minutes once every two or four weeks. When given with Yervoy (ipilimumab) or chemotherapy, it is usually given once every two, three, or four weeks.
Keytruda (pembrolizumab) is injected over 30 minutes every three or six weeks.
Imfinzi (durvalumab) is injected over 60 minutes every two, three, or four weeks.
Tecentriq (atezolizumab) is injected over 30 to 60 minutes every two, three, or four weeks.
Yervoy (ipilimumab) is injected over 30 minutes once every six weeks.
Imjudo (tremelimumab) is injected over 60 minutes every three weeks for four doses (cycles 1 to 4) and then as a single dose at week 16 (cycle 6).
Immunotherapy is often given in combination with several other types of therapy, including surgery, chemotherapy, radiation, or targeted therapies. They may also be combined with other immunotherapies that work in different ways. Different immunotherapies have been approved for each type of cancer.
The chosen approach depends on:
Cancer stage
If the tumor can be removed surgically
If you’re healthy enough for chemotherapy
If cancer has responded to previous treatments
If it has come back after treatment
NSCLC Immunotherapy
Immunotherapy treatments for non-small cell lung cancers include the following:
Opdivo may be used with chemotherapy as a first treatment before surgery.
Tecentriq may be used after surgery for some stage 2 and stage 3 cancers.
Tecentriq or Keytruda may be used in people with earlier stages after surgery and chemotherapy.
Keytruda or Libtayo may be the first treatment for stage 3 cancers that can’t be taken out with surgery or in people not healthy enough for chemotherapy with radiation.
Imfinzi may treat stage 3 cancer that cannot be removed with surgery and has not gotten worse after chemotherapy with radiation.
Imfinzi may be used on stages 3A, 3B, and 3C cancers after chemotherapy and radiation.
Keytruda, Tecentriq, or Libtayo may be used (sometimes with chemotherapy) as part of the first treatment in some people with stage 4 cancers.
Opdivo plus Yervoy may be part of the first treatment for stage 4 cancers.
Imfinzi and Imjudo may be part of the first treatment for stage 4 cancers, typically with chemotherapy.
Opdivo, Keytruda, and Tecentriq may treat certain types of advanced cancers that come back after initial treatments.
Keytruda or Tecentriq, with or without chemotherapy, may be used for new stage 4, relapsed, and recurrent cancers.
Opdivo, Keytruda, or Tecentriq may be used for stage 4 cancers that are getting worse or relapsed.
SCLC Immunotherapy
Immunotherapy treatmenta for small cell lung cancers include the following:
Tecentriq and Imfinzi may be used along with chemotherapy as the first treatment for advanced cancers.
Tecentriq and Imfinzi can also be continued alone to slow cancer progression.
Tecentriq and Imfinzi may be used to treat cancer that has come back after treatment.
Mesothelioma Immunotherapy
Immunotherapy treatments for mesothelioma include the following:
Keytruda and Opdivo may treat cancers that are still growing after initial treatment.
Yervoy may be used along with Opdivo to treat advanced cancers.
Yervoy and Opdivo may also be the first treatment for cancers that cannot be removed with surgery.
Lung Cancer Stage and Immunotherapy Success Rate
While many immunotherapies are still relatively new treatments, they have significantly impacted treatment plans for lung cancers.
Generally, studies of lung cancers have shown that immunotherapy leads to considerable improvement in the person treated. Sometimes, these treatments are preferred over traditional treatments, even as a first treatment option.
Other studies have shown that immunotherapy has helped even people with advanced lung cancers live longer than expected—including taking these drugs for many years, leading to long-lasting remissions and longer survival rates.
Oncologists (cancer specialists) treating lung cancer with immunotherapy have seen people doing well, with no sign of cancer, five years or more after their initial treatment. For example, 80% of people with early-stage non-small cell lung cancer treated with Opdivo and surgery survived after five years. In contrast, five-year survival rates from standard treatments are between 36% and 68%.
A phase 3 trial of Opdivo plus chemotherapy (followed by surgery) on stages 1B to 3A non-small cell lung cancers showed that people getting both immunotherapy and chemotherapy lived longer without their cancer worsening. Survival rates averaged 31.6 months compared to 20.8 months for those who had only chemotherapy before surgery.
Another phase 3 clinical trial compared Opdivo plus Yervoy with chemotherapy in stage 4 or recurrent cancers. People getting immunotherapy responded better to treatment and lived longer without their cancer worsening.
Forty-three percent of people taking immunotherapy had not seen their cancer get worse in one year, compared to just 13% with chemotherapy. Sixty-eight percent of people who responded to the immunotherapy were still doing well at one year, compared to just 25% on chemotherapy.
Not all people see the same results from immunotherapies. Some need to stop the drugs because of side effects or adverse reactions. Some people’s cancer keeps growing even after immunotherapy treatment.
Every stage and type of lung cancer has different treatment options and survival rates. Immunotherapy is not necessarily an option for all lung cancers, and every person will have a different experience with their treatment. Doctors are still studying how best to use these drugs and which cancers are best suited to them.
Related: Is Lung Cancer Curable? Treatment Options and Survival Rate
Side Effects of Immunotherapy
Side effects of immunotherapy are typically milder than those that come with chemotherapy. It varies by the type of immunotherapy. With any of them, more serious reactions can happen during or after infusions.
The risk of side effects and reactions increases if two types of immunotherapy are combined.
Immunotherapy side effects include:
Fatigue
Cough
Nausea
Itching
Skin rash or other reactions
Loss of appetite
Constipation
Joint pain
Diarrhea
Muscle or bone pain
Belly pain
Flu-like symptoms
Shortness of breath from lung inflammation
Weight changes
Other, more severe side effects occur less often. An infusion reaction may occur after the IV infusion of these drugs. Infusion reactions come on suddenly and can cause:
Fever
Chills
Flushing of the face
Rash
Itchy skin
Feeling dizzy
Wheezing
Trouble breathing
Tell the healthcare providers immediately if you start having these symptoms at the clinic.
Immunotherapy can sometimes lead to autoimmune reactions because the immune system checkpoints are essential in keeping your immune system from overreacting to your body’s normal, healthy cells.
This reaction can cause severe or life-threatening problems in the lungs, intestines, liver, endocrine glands, kidneys, or other organs.
Make sure to mention any new side effects to your oncologist. They may mean you must stop immunotherapy and get other medicines to reduce damage to your other organs.
Talk to your healthcare provider if you have any symptoms or side effects, even if you think it isn’t relevant or related. Even if you’ve mentioned a sign before, tell the team about any changes in your health. Your care team or palliative care team can help treat your side effects.
Self-Care on Immunotherapy
Taking care of your body is essential for immunotherapy or cancer treatment. Eat a healthy diet focusing on fruits, veggies, low-fat foods, and protein-rich snacks. Avoid high-fat animal products and salty foods.
While getting immunotherapy, you may feel extra tired. Listen to your body and rest when you need to. Ask your friends and family to pitch in so you can take it easy.
Keep your body strong and your weight up by eating enough healthy foods. Light exercise can help with fatigue and nausea when you feel up to it. Try walking for short periods and stay hydrated.
If you have digestive distress while on immunotherapy, take these steps to improve this side effect:
Avoid caffeine and alcohol.
Avoid hot, spicy foods.
Stay away from overly sweet or greasy foods.
Drink lots of water and other clear liquids.
Eat small, frequent meals. Try splitting your food intake into 6 to 8 smaller meals.
Eat dry foods such as crackers or dry cereal.
Follow-ups With Your Oncologist
During immunotherapy, you’ll meet regularly with your care team. They’ll order tests to monitor your health and treatment plan. Tell them about any new side effects or symptoms. You may consider asking some additional questions about your immunotherapy, including:
Are there any medicines I should not take?
Are there any other medicines I should keep on hand?
What over-the-counter medicines am I allowed to take?
Are there any vitamins and supplements I should or should not take?
Do I need to use birth control? What should I do if I want to get pregnant in the future?
What should I do if I get a rash?
If my skin or eyes are itchy, what can I use to treat this?
What can I do about my fatigue?
When should I call the doctor?
Am I at risk for infections?
Are there any foods I should avoid so as not to get an infection?
Is it OK to be in a crowd of people? Do I have to wear a mask?
Can I have visitors over? Do they need to wear a mask?
Am I at risk for bleeding? What should I do if I cut myself or start bleeding?
Summary
Immunotherapy is a newer class of treatment for lung cancer. It works by boosting the body's immune system to fight cancer. The three main types of immunotherapy for lung cancer are checkpoint inhibitors, cancer vaccines, and CAR T-cell therapy. Only checkpoint inhibitors immunotherapy is FDA-approved for use on lung cancers. The others are still in clinical trials.
Checkpoint inhibitors block proteins that help cancer cells evade the immune system. Common checkpoint inhibitors for lung cancer include pembrolizumab (Keytruda), nivolumab (Opdivo), and atezolizumab (Tecentriq).
They can treat different stages of lung cancer. These include early-stage, advanced-stage, and recurrent cancer. They are often used with other treatments, such as surgery, chemotherapy, and radiation therapy. The success rate of immunotherapy for lung cancer varies depending on the type of cancer and the cancer stage.
Immunotherapy is often given as an infusion into a vein. These infusions can take 30 to 60 minutes on a set schedule. Immunotherapy can have side effects, such as fatigue, rash, and diarrhea. The side effects of immunotherapy can be mild or severe and vary from person to person.
Immunotherapy can cause severe reactions during or after infusions. These include infusion reactions and autoimmune reactions.
Read the original article on Verywell Health.

