What Is Acute Myeloid Leukemia?
A Rare and Aggressive Blood Cancer
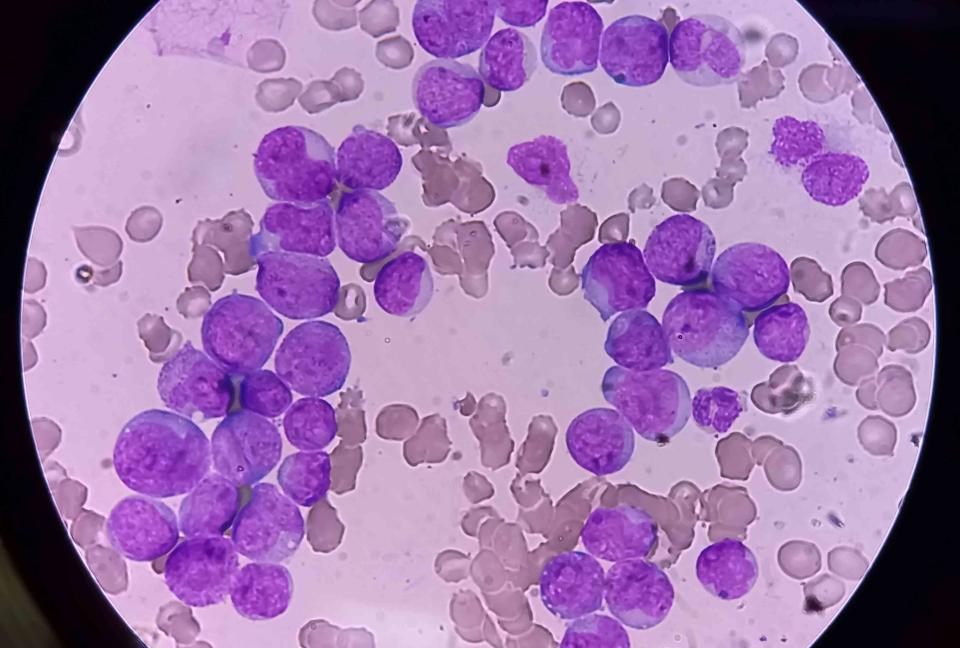
Md Babul Hosen / Getty Images
Medically reviewed by Doru Paul, MD
Acute myeloid leukemia (AML) is a rare blood cancer. It begins when the bone marrow cells that usually make blood cells start producing immature white blood cells called myeloblasts. It may be referred to as acute myelogenous leukemia or acute nonlymphocytic leukemia.
Myeloblasts infiltrate the bone marrow and blood, causing symptoms that worsen quickly if it is not treated. The cancer can spread to the lymph nodes, spleen, liver, brain, spinal cord, skin, gums, and testicles.
AML is aggressive and rare. It accounts for about 1% of cancer cases yearly. It was predicted that about 20,380 people would be diagnosed with AML in 2023 and about 11,310 people with AML would die in 2023, making up about 1.9% of all cancer deaths. AML commonly affects older adults (over 65 years), and adults account for almost all deaths from it.
This article will explain the symptoms and treatment options for acute myeloid leukemia and include information about life expectancy and survival rates.
Acute Myeloid Leukemia Symptoms
The symptoms of acute myeloid leukemia are often confused with other illnesses. Most often, these symptoms are seen in other, more common diseases.
Often, the earliest sign of AML is feeling fatigued. Other symptoms of AML can include:
Looking pale
Frequent infections
Having fevers without a known cause
People with a type of AML called acute promyelocytic leukemia have trouble with bleeding and blood-clotting—nosebleeds, cuts that don’t stop bleeding, and blood clots in the legs or lungs.
As the leukemia cells take over the bone marrow and blood, they crowd out other blood cells (red blood cells, white blood cells, and platelets), causing complications. These complications can also cause symptoms.
These include:
Low red blood cells (anemia) can make you feel tired, weak, cold, dizzy, and light-headed and cause headaches, pale skin, and shortness of breath.
Low white blood cells (neutropenia) can leave you open to infections.
Low platelets (thrombocytopenia) can lead to bruises and excessive bleeding in the form of nosebleeds, bleeding gums, and heavy menstrual periods.
High numbers of leukemia cells clogging blood vessels (leukostasis) can cause headaches, one-sided weakness, slurred speech, confusion, sleepiness, bone or joint pain, and an enlarged spleen.
As AML advances, it can spread to other areas of the body. It can form tumor-like collections of leukemia cells called chloroma, granulocytic sarcoma, or myeloid sarcoma. The spread of AML can cause symptoms that include the following:
Lumps or rashes in the skin
Swelling, pain, and bleeding of the gums
Cancer reaching the brain and spinal cord can cause headaches, weakness, seizures, vomiting, clumsiness, facial numbness, and blurry vision
Enlarged lymph nodes in the neck, groin, underarm areas, or above the collarbone, which may be felt as lumps under the skin
Related: Chronic Myeloid Leukemia vs. Chronic Lymphocytic Leukemia: What Are the Differences?
What Causes AML?
It’s hard to know what causes AML. Certain factors can increase a person’s risk of developing this cancer, but AML has no known cause in most cases.
Specific genetic changes can lead bone marrow cells down a cancerous road. Often in cases of AML, these changes build up over a person’s lifetime. In a few cases of AML, people inherit gene changes that make them more likely to get this cancer.
Risk Factors for AML
Several factors increase your risk of developing AML. It’s more common in older people, males, and those with a family history of AML. (Note that the terms for sex or gender from the cited source are used in this article.)
Smoking and chemical exposures, including benzene, formaldehyde, chemotherapy drugs, or radiation, also increase risk. People with blood disorders like myelodysplastic syndrome (MDS) or some genetic syndromes are at an increased risk of developing AML.
How to Detect Acute Myeloid Leukemia
If a healthcare provider suspects AML, they’ll do an initial exam and take your health history as the first step toward an AML diagnosis. They will closely examine your mouth, eyes, skin, liver, lymph nodes, spleen, and nervous system. They’ll also ask about or look for bruising or bleeding and ask about infections you have had recently.
They will request blood testing from the lab, which may include the following:
Complete blood count (CBC) of the amounts of different cells in the blood
Peripheral blood smear to look for myeloblasts in the blood under the microscope
Blood chemistry tests to check your overall health and the function of many vital organs
Coagulation tests to check how the blood clots
The healthcare provider will also order imaging tests to see what’s happening inside your body. These may include:
X-rays for lung infections
Computed tomography (CT) scan before a biopsy (removing a sample tissue for analysis in a lab) or to learn where cancer may be growing
Magnetic resonance imaging (MRI) to examine the brain and spinal cord
Ultrasound to examine the lymph nodes
They’ll likely perform a bone marrow aspiration or biopsy, sampling the spongy bone marrow tissue inside the bones. They’ll look at what percentage of bone marrow cells are myeloblasts. For a diagnosis of AML, the blood or bone marrow needs to be at least 20% myeloblasts. In normal bone marrow, they are 5% or less.
You may need to have a sample of your spinal fluid collected via lumbar puncture if your healthcare team suspects the cancer has spread to the nervous system.
To understand your type of the AML better, they’ll do genetic and chromosomal testing on your bone marrow or blood samples. They may also analyze the samples using dyes and antibodies to classify the cancer.
Related: AML vs. CML: What Are the Differences?
Treatment Options for Acute Myeloid Leukemia
Acute myeloid leukemia is treated with a combination of medicines and procedures. These include chemotherapy, radiation therapy, stem cell transplants, and targeted therapies.
Treatment is typically done in two phases. The first, sometimes called remission induction therapy, is intense and aimed at destroying as many leukemia cells as possible. Typically this involves chemotherapy and targeted treatments, depending on the person's general health and age.
Once the person has responded, a remission phase of treatment begins. After a person's remission, treatments are less intense but aim to kill any remaining cells. Called postremission or remission continuation therapy, the aim is to keep any leukemia cells from growing and causing a relapse.
During this time, a stem cell transplant may be an option to replace a person's blood-making cells with those from another healthy person.
Chemotherapy kills fast-growing cells, including cancer cells. It is used in high doses during the remission induction phase and in lower doses for remission continuation therapy. Chemotherapy drugs are often used in combinations, sometimes with targeted treatments.
Targeted treatments specifically destroy cancer cells based on the cancer's characteristics. These include:
Mylotarg (gemtuzumab ozogamicin) is a toxic substance linked to an antibody that binds to CD33, a protein in some leukemia cells.
Rydapt (midostaurin) is a protein kinase inhibitor used for AML with a mutation in the FLT3 gene.
Xospata (gilteritinib) is a tyrosine kinase inhibitor for AML that has come back or did not get better with other treatments and has a mutation in the FLT3 gene.
Vanflyta (quizartinib) is a tyrosine kinase inhibitor used for AML with a mutation in the FLT3 gene.
Less-intensive targeted therapies may be used in people who cannot receive other treatments. These include:
Daurismo (glasdegib) for adults over 75 or with health issues that are newly diagnosed with acute myeloid leukemia
Tibsovo (ivosidenib) for AML with a mutation in the IDH1 gene
IDHIFA (enasidenib) for AML with a mutation in the IDH2 gene
Other drugs, like arsenic trioxide and all-trans retinoic acid, can treat AML subtype acute promyelocytic leukemia.
If their red blood cells or platelets get too low, people with AML may also need blood transfusions and other treatments. Antivirals and antifungals can treat and prevent infections.
Related: Acute Myeloid Leukemia: Treatment for Relapsed or Refractory Disease
What Is the Prognosis for Acute Myeloid Leukemia?
The prognosis for people with acute myeloid leukemia is not great. AML is the 14th deadliest cancer. One subtype, acute monocytic leukemia, is even more deadly and is the 13th most fatal cancer.
The percentage of people diagnosed with AML who are still alive five years later was 31.7% between 2013 and 2019. Older people are harder hit with this disease than younger people. For people diagnosed after the age of 20, only 28% are alive five years later. But for people younger than 20, 69% are still alive.
These statistics do not represent individual cases, and many of the targeted drugs have only recently been approved and added to AML treatment regimens. Age-adjusted death rates have been falling on average 0.6% each year between 2011 and 2020.
In addition to age, the survival rates for AML vary based on several factors. These include a person’s general health, how well their treatments work, the AML subtype, and the genetic changes the cancer cells have. Most people over 20 have less than five years of life after an AML diagnosis.
Acute promyelocytic leukemia (APL) is a unique subtype of AML that represents approximately 5% to 20% of all cases of adult AML (600 to 800 new cases per year). Due to advances in the diagnosis and treatment of this disease, APL is now considered the most curable form of adult leukemia. Cure rates of 90% and more have been reported from centers specialized in AML treatment.
Related: Acute Myeloid Leukemia Survival Rates and Outlook
Summary
Acute myeloid leukemia (AML) is a rare and aggressive blood cancer. If left untreated, AML can quickly spread. It primarily affects older adults over the age of 65.
The symptoms of AML are often mistaken for other illnesses. They include fatigue, swollen lymph nodes, pale appearance, frequent infections, unintentional weight loss, fevers without a known cause, night sweats, and loss of appetite
Complications can arise as the leukemia cells multiply and replace healthy blood cells. These include anemia, neutropenia, thrombocytopenia, and leukostasis. AML can also spread to other body areas, leading to symptoms.
Diagnosing AML involves physical exam, blood tests, imaging tests (such as X-rays, CT scans, MRI, and ultrasound), bone marrow testing, and genetic and chromosome testing
Treatment for AML typically involves chemotherapy, radiation therapy, stem cell transplants, and targeted therapies. Sometimes, blood transfusions and antiviral or antifungal medications may also be necessary.
The prognosis for AML is generally poor, with AML ranking as the 14th deadliest cancer. The five-year survival rate for AML between 2013 and 2019 was 31.7%. Older people have a lower survival rate than younger individuals. Factors like general health, treatment efficacy, and specific genetic mutations play a role in determining individual prognosis. However, acute promyelocytic leukemia now has a very good prognosis due to treatment advances.
Read the original article on Verywell Health.

