Actinic Keratosis vs. Basal Cell Carcinoma: Differences and Similarities
Medically reviewed by Gagandeep Brar, MD
Basal cell carcinoma is the most common form of nonmelanoma skin cancer. In contrast, actinic keratosis is a precancerous condition that sometimes turns into skin cancer.
If you have actinic (solar) keratosis (AK) lesions, you are at a heightened risk for two types of skin cancer: basal cell carcinoma (BCC) and squamous cell carcinoma. Actinic keratosis is more likely to progress into squamous cell carcinoma (SCC) than BCC.
This article will discuss the differences in appearance between actinic keratosis and basal cell carcinoma. It will also detail the causes and treatments for both conditions.
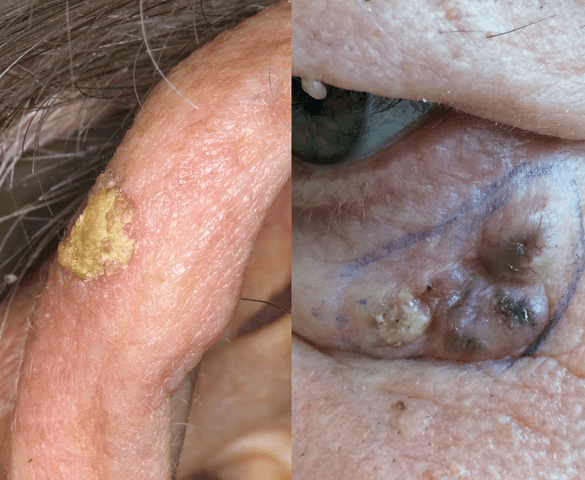
Reproduced with permission from © DermNet dermnetnz.org 2023
Actinic keratosis on ear and basal cell carcinoma under eyeHow Actinic Keratosis and Basal Cell Carcinoma Look
Basal cell carcinomas have been known to be misdiagnosed as AK lesions, though this is rare. In general, these conditions don't resemble each other physically.
If you suspect you have one or more AK or BCC lesions, a specialist, such as a dermatologist, may make a preliminary diagnosis by examining your skin. To do this, they may view the lesions and surrounding areas of skin noninvasively with a magnifying lens called a dermatoscope.
AK and BCC may have the following characteristics:
Actinic Keratosis
Small size
Scaly, rough, or crusty texture
Red, tan, white, pink, or flesh-toned in color. In some instances, several colors may appear within one patch
Can be raised or flat
May feel dry to the touch
Basal Cell Carcinoma
Open sores that don’t heal for weeks or months, or that reemerge after healing; may bleed, ooze, or crust
Red, irritated patches of skin that are painful or itchy
Small, shiny bumps that vary in color, including being tan, brown, or black in dark-skinned people or pink, red, white, or clear in light-skinned people
Tiny pink growths with raised, rolled edges and crusted, indented centers that may have visible surface blood vessels
Scar-like areas of skin that have poorly defined borders that may look shiny or waxy
Positive Pathology Findings
Basal cell carcinoma and actinic keratosis are definitively diagnosed through a biopsy (removing a sample tissue for examination in the lab). These conditions do not resemble each other under a microscope.
To get a skin sample to biopsy, part or all of the suspicious lesion will be removed for laboratory analysis. If you have multiple lesions, samples may be taken from some or all.
A pathologist will analyze the skin samples under a microscope, to check for evidence of cancer. If cancer cells are found, these findings are said to be positive for cancer.
The pathologist will also use the skin samples to determine if you have a different diagnosis, rather than skin cancer or AK. Conditions that mimic skin cancer include benign moles (nevus) and psoriasis.
Differences and Similarties Between BCC and SCC
Basal cell carcinomas and squamous cell carcinoma most commonly affect areas of unprotected skin that have been exposed consistently to sunlight.
BCC and SCC are both forms of nonmelanoma skin cancer. Both types may spread into nearby tissues when they're not caught early. Neither type is likely to metastasize into distant regions of the body.
Around 75% to 80% of nonmelanoma skin cancer is basal cell carcinoma. These skin cancers start in basal cells located in the outermost layer of the skin.
Around 20% of nonmelanoma skin cancer is squamous cell carcinoma. These skin cancers start in squamous cells located in the outer or middle layers of the skin.
SCC is faster-growing than BCC. It is also more likely to spread into nearby tissues or grow deeply into the skin's inner layers.
Actinic Keratosis Progressing to Basal Cell Carcinoma
Not every AK lesion becomes cancerous. Around 1% to 10% of AK progresses to SCC. Actinic keratosis may also transform into basal cell carcinoma, but this is less common.
The transformation of actinic keratosis into squamous cell carcinoma is thought to be faster than the progression of AK into basal cell carcinoma. Both transformations may take up to two years.
Sun Exposure: Actinic Keratosis vs. Basal Cell Carcinoma
Long-term sun exposure of unprotected skin is the main risk factor for basal cell carcinoma and actinic keratosis. That's why these lesions typically manifest on the face and on areas of the body that get the most sun.
If you don't protect your skin with sunscreen containing a high sun protection factor (SPF), clothing, or hats, you may be putting yourself at risk for all types of skin cancer, including malignant melanoma, the deadliest form. Outdoor workers, exercisers, and sunbathers are all vulnerable populations.
Since damage from the sun's ultraviolet (UV) rays is cumulative, older adults are at a heightened risk. However, anyone of any age can get skin cancer.
Other Causes
In addition to the sun, exposure to UV radiation from human-made sources can put you at risk for precancers and cancers of the skin. These include:
Tanning beds, tanning booths, and sunlamps
Black-light lamps
Additional Risk Factors
Anyone can get skin cancer. However, certain risk factors may make you more vulnerable:
Being older
Light skin tone
Blue or green eyes
Blond or red hair
Having skin that burns, reddens, or freckles easily
Having many moles
Family or personal history of skin cancer
Living in a geographic area where sunlight is strong and prevalent throughout all or most of the calendar year
Treatment Differences
The treatment options for these conditions have some overlap but may vary. When your treatment plan is being determined, several factors will be considered, including your personal preferences, age, and general health.
The size, location, and number of lesions you have will also be a factor. In general, BCC is treated more aggressively than AK, especially if it has spread.
Precancerous Actinic Keratosis
It's not possible to predict which AK lesions will become cancerous and which won't, so destroying or removing the lesion or lesions is typically recommended. You may also wish to have AK lesions removed for cosmetic reasons, or to eliminate symptoms, like itching or pain.
Some AK treatments may be done in one or two sessions at a dermatologist's office. They include:
Cryosurgery: This procedure uses liquid nitrogen or another freezing substance to freeze off the AK lesion within a few days. One or two sessions may be needed before results are seen.
Chemical peel: Unlike cosmetic chemical peels, this medical-grade peel completely destroys and eradicates the top layer of treated skin.
Curettage: Thick or deep AK lesions may be removed via curettage. During the procedure, AK is scraped out of the skin with a tool called a curette. The scraped area may then be treated with heat (electrodesiccation) to destroy any remaining cells.
Photodynamic therapy: This treatment is typically used on recurring AK lesions. Your dermatologist will apply a solution to your skin, which will remain in place for an hour or longer. The solution will then be activated with blue or red light. A follow-up treatment is usually done three weeks later.
Laser resurfacing: AK lesions on the lips (actinic cheilitis) are often treated with laser resurfacing. During this treatment, the surface layer of the lesion will be removed via a laser so that new, healthy skin can emerge.
If you have many AK lesions or lesions that can be felt but not seen, your dermatologist may recommend at-home treatment instead of an in-office procedure. You will apply topical medication for several weeks or longer. Medications used for this purpose include:
Voltaren (diclofenac sodium) gel, a nonsteroidal anti-inflammatory drug (NSAID)
Efudex or Carac (5-fluorouracil) cream, a topical chemotherapy drug
Aldara (imiquimod) cream, an immune response modifier
Klisyri (tirbanibulin) ointment, a microtubule inhibitor (targets dividing cells)
Cancerous Basal Cell Carcinoma
Several treatments are used to eradicate BCC tumors. Surgical removal is often recommended. The surgical procedures most commonly used for BCC are:
Curettage and electrodesiccation: This procedure is also done to remove AK lesions.
Wide-local excision: During this procedure, the tumor plus a surrounding margin of healthy tissue will be cut out (surgically removed).
Mohs surgery: Your surgeon will painstakingly remove very thin layers of skin, one at a time, to examine for cancerous cells. This procedure produces minimal scarring, so it is often done to treat BCC lesions on the face.
Other treatments may be recommended if you aren't a candidate for surgery or have very superficial BCC lesions. They include:
Radiation
Cryotherapy
Topical chemotherapy
Photodynamic therapy
Immune response modifiers
Targeted therapy
Immunotherapy
Risks of Untreated Symptoms
AK may progress into squamous cell carcinoma or basal cell carcinoma. When left untreated, these skin cancers can cause disfigurement, as well as discomfort. SCC can also, in some instances, become deadly.
Always have a specialist, like a dermatologist, assess any lesions you have on your skin. They can best determine if treatment is needed and, if so, which kind makes sense for you.
Summary
Actinic keratosis is a precancerous condition that sometimes progresses into skin cancer. It is most likely to transform into squamous cell carcinoma. It may also transform into basal cell carcinoma.
AK lesions do not typically resemble basal cell carcinoma visually or under a microscope. A dermatologist can diagnose both conditions and guide you towards the best treatment option.
Read the original article on Verywell Health.