7 Signs You Could Have Mumps

Mumps is a contagious viral infection that affects your salivary glands. It used to be pretty common in the past until the MMR vaccine (which protects against measles, mumps, and rubella) became a standard childhood vaccination in the U.S. in 1967. Nevertheless, it’s still possible to get mumps, especially if you live or work in an environment where close contact with other people happens frequently or is unavoidable (like schools).
“Mumps is a respiratory virus that spreads through contact with saliva or respiratory secretions,” Amesh Adalja, MD, an emergency medicine and infectious disease doctor who is a senior scholar at the Johns Hopkins University Center for Health Security, tells Health.
This means that you can get mumps if you come in contact with the saliva or mucus of an infected person—usually through coughing and sneezing. “Large outbreaks at college campuses—there is one now at Temple University—suggest that vaccine-induced immunity wanes with age,” Dr. Adalja says. “Mumps is now…more common in young adults (which is also the result of exposure pressure in crowded dormitory environments).”
RELATED: 5 Things You Must Know About Mumps Even If You Got the Vaccine
Mumps symptoms
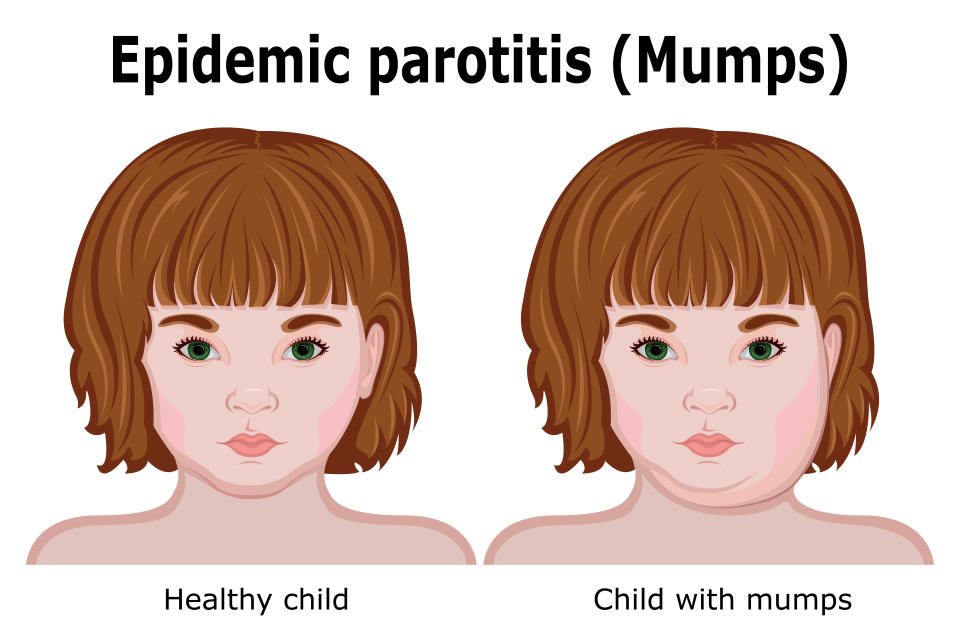
So what do mumps look like? It’s a very distinctive infection, because It causes your cheeks and jaw to swell and look puffy.
“Mumps is characterized by swelling of the parotid salivary glands, which give a patient with mumps a very specific appearance in which their face is swollen,” Dr. Adalja says.
Other common signs of mumps include:
Fever
Headache
Muscles aches
Loss of appetite
Dry mouth
The symptoms of mumps in adults are basically the same as those in teens and children. It’s also very possible to not experience any mumps symptoms, or very mild ones, while infected.
RELATED: 5 Old-Time Diseases That Are Making a Comeback
Rarer signs of mumps
“In up to 10% of mumps cases in males, swelling of the testes (orchitis) can occur,” Dr. Adalja says. Women with mumps may experience swelling of the ovaries (oophoritis), although it's also uncommon. “Other rare mumps complications can include pancreatitis, meningitis, and encephalitis,” he adds.
Both meningitis (inflammation of the membranes that cover the brain and spinal cord) and encephalitis (inflammation of the brain) are very concerning. “If a person develops a stiff neck, trouble concentrating or thinking, severe headaches, or seizures, a dangerous complication could be present,” Dr. Adalja says.
RELATED: 7 Things You Need to Know About Vaccines
What to do if you suspect you have mumps
Mumps symptoms tend to appear a couple of weeks after exposure to the virus—anywhere from 12 to 25 days, according to the CDC. It’s also possible to have the virus and experience no mumps symptoms at all.
If you notice any mumps symptoms in yourself or your family, contact a doctor immediately. Before going in to the hospital or doctor’s office, it’s important that you disclose in advance that you suspect mumps so that preparations can be made to prevent the spread of the infection to other people during your visit.
There’s no particular medication for the mumps virus. Instead, treatment is focused on alleviating mumps symptoms until the infection runs its course—which usually happens within a few weeks, according to the CDC.
While waiting for that to happen, your doctor will likely recommend that you:
Take painkillers to relieve any pain and bring down your fever.
Drink plenty of fluids, particularly water, to stay hydrated.
Apply a warm or cold compress to your swollen salivary glands.
Avoid acidic foods, fruits, and drinks.
Get plenty of rest.
Avoid foods that require a lot of chewing.
RELATED: A 6-Year-Old Unvaccinated Boy Spent 57 Days in the Hospital for Tetanus—and Racked Up an $800K Bill
How to prevent mumps
The most effective way to prevent mumps is to get vaccinated against it. If you haven’t already received the standard two doses of the MMR vaccine as a kid, you should receive at least one dose of the vaccine. Your doctor may recommend that you receive two doses if you live or work in environments like colleges where close contact is inevitable. In outbreak settings, a third dose is often administered.
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
