Questions Swirl Around the Procedure That Led to Joan Rivers' Death
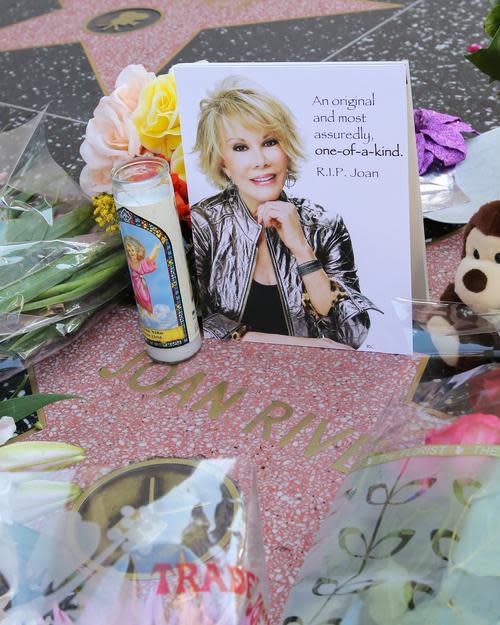
A memorial tribute on the Hollywood Walk of Fame. Photo by Paul Archuleta/Getty Images
As the New York State Health Department launches an investigation, questions remain about the circumstances leading to Joan Rivers’ death last week. The tragedy began when Rivers, 81, lost consciousness at an outpatient surgery clinic in Manhattan during an elective vocal cord procedure and was then rushed six minutes across town to Mount Sinai Hospital for emergency care. And while it might take some time before the public knows more about what happened, Yahoo Health checked in with some experts regarding protocol for treating elderly outpatients in settings such as Yorkville Endoscopy, where Rivers had her ill-fated procedure (and which could not be reached for comment). And, surprisingly, age is not the most important factor when assessing risks.
“With the elderly—unlike with kids—there aren’t specific milestones at specific ages,” Dr. John Abenstein, president-elect of the American Society of Anesthesiologists, told Yahoo Health. “I can have a 50-year-old patient, for example, who is physiologically older than an 80-year-old.”
Related: Joan Rivers’s Funeral Set for Sunday; Burial Arrangements Underway
Abenstein, who practices anesthesiology at an outpatient clinic that’s affiliated with the Mayo Clinic in Minnesota, said he routinely takes care of patients 90 and older, and that doing so is common at outpatient centers across the country. “It can be done safely under many circumstances,” he noted, adding that what’s most important is assessing a patient’s underlying health status, functional status, medical history, and the risk factors of the procedure itself.
One of the first questions he asks patients when deciding whether to move forward with a sedated procedure is if they can walk up two flights of stairs. “If the answer is ‘yes,’ it’s most likely appropriate,” he said. If the answer is “no,” he dives deeper to uncover why—to find out if it’s because of arthritis, for example, or a cardiovascular issue, which could be a red flag. “Cardiopulmonary function is what we concentrate most on,” he added. That’s because the highest risk with anesthesia in general, he said, relate to the depth of sedation, and the fact that the deeper one is put under, the harder it is to breathe and protect oneself with reflexes (the gag reflex, for example).
Related: Are You Getting the Right Anesthetic?
While no official details have been released regarding what, if any, anesthesia was administered to Rivers, some sources have pointed to Propofol, the drug connected to the death of Michael Jackson. “The advantage of Propofol,” Abenstein said, “is that it’s very short-acting, and the patient can wake up faster.” The risks are that it’s a “tricky drug to use,” because it can be difficult to find the perfect dose to keep a person breathing but not writhing around.
As for outpatient vs. in-hospital procedures requiring sedation, “The biggest risk in an outpatient setting is the depth of resources available if a patient’s condition changes,” Abenstein explained. Oftentimes, he said, the only emergency plan is to call 911.
Related: Four Tests Worth Getting at the Doctor’s Office
It’s why Kevin Campbell, a cardiologist and heart-rhythm disorder specialist based in North Carolina, told Yahoo Health he was often wary of outpatient anesthesia-based procedures. “I prefer older patients with risk factors to have procedures done in a hospital, just in case,” he said. “Sometimes in an outpatient setting it’s a different mindset, and I worry that they sometimes cut corners.”
Still, he agreed that it was often appropriate for an elderly individual to undergo an anesthetized procedure in an outpatient clinic. “It depends on the procedure,” Campbell said. “If it’s a low-risk elective surgery, with low-risk sedation, and various criteria are met, then it’s probably acceptable.”
Related: 5 Lies You’ve Been Told About Your Own Body
Before submitting to the operation, he advised, a person “should be evaluated by a primary-care doctor and get pre-op clearance from a cardiologist.” It’s also advisable for patients to find out as many details as possible regarding the clinic’s plan for administering the anesthesia— what sort it will be, what the possible risks and side effects are, what the emergency plan is in case something goes wrong, and even who will be administering the sedation.
“Will it be a nurse anesthetist? That’s fine, but there should at least be a board-certified anesthesiologist on the premises,” Campbell said — a rule Abenstein wholeheartedly agreed with.
Read This Next: Miss Colorado Gets Real About Why Nurses Are So Amazing

