Should You Worry About Rising Mpox Cases?
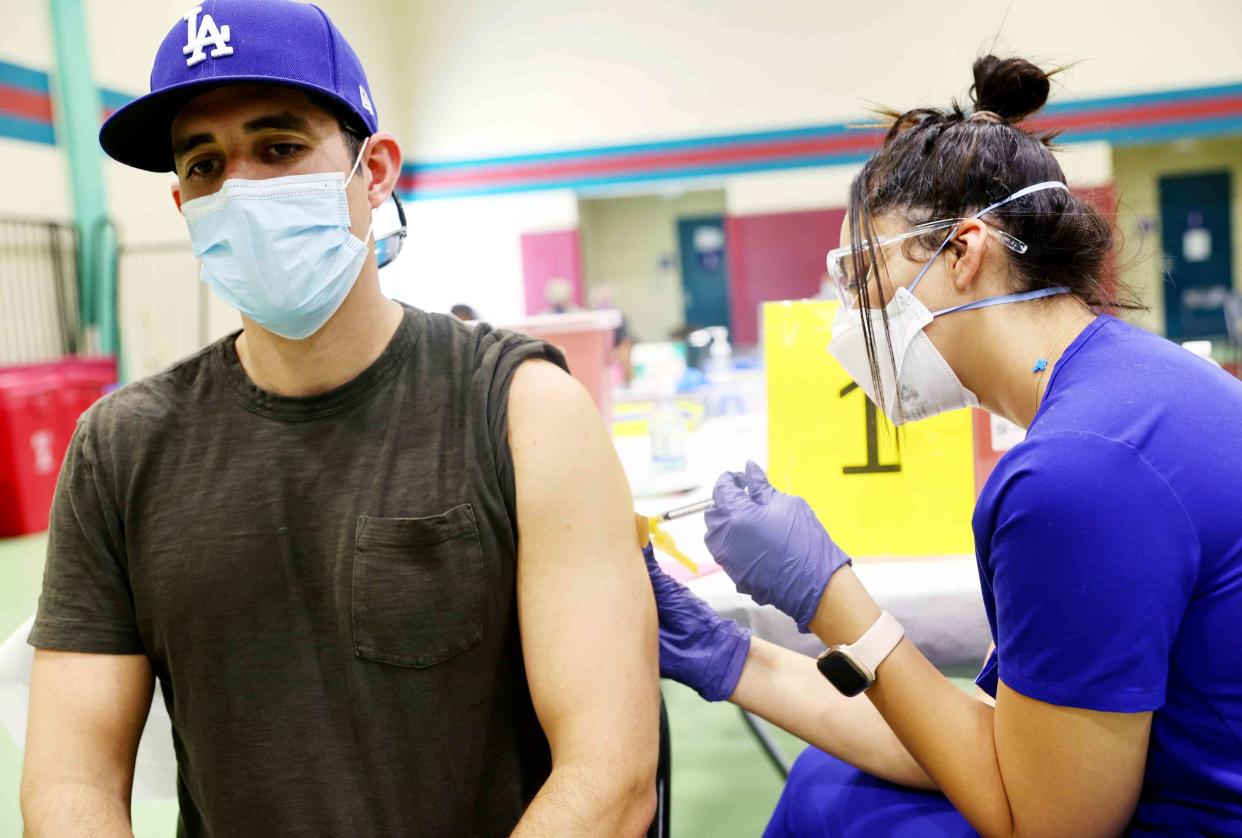
Mario Tama / Staff / Getty Images
Fact checked by Nick Blackmer
Key Takeaways
Mpox cases are rising in the United States, albeit not reaching the peak levels in 2022.
Experts say that it’s unclear what's driving the uptick in cases.
Jynneos, a vaccine for mpox, is available for at-risk people.
Mpox cases appear to be rising in the United States again.
The Centers for Disease Control and Prevention (CDC) has recorded 656 mpox cases in 2024 so far, doubling the 2023 figure of 306 in the same period. As of March 30, the states with the most infections were New York, California, New Jersey, and Illinois.
While levels are nowhere near the 32,000 cases in the 2022 mpox outbreak, keeping up to date with prevention strategies can help keep you healthy if you’re at risk for mpox.
Related: An Mpox Patient Told Us How He Navigated Testing, Treatment, and Recovery
Why Are Mpox Cases Going Up Again?
The reason for the uptick in cases is unclear, said Andrew Noymer, MSc, PhD, an associate professor of population health and disease prevention at the University of California-Irvine. A few factors could be at play: the disease is endemic, identification rates are lower, and vaccination rates have been declining.
Noymer said mpox tends to stay “in social networks” rather than the population at large because it “requires skin-to-skin contact and not airborne transmission.” The virus isn’t technically considered a sexually transmitted infection (STI), but much of its transmission has been due to sexual and intimate contact.
Related: Should Mpox Be Called an STI?
Mpox is caused by a virus in the same family as smallpox. Its symptoms include swollen lymph nodes, muscle aches, and fever, as well as a characteristic rash and skin lesions that scab over as they heal. Skin contact with these rashes and scabs can spread mpox, as can bodily fluids.
While the rising number of cases is a cause for concern, experts say the numbers aren't as worrying as the previous outbreak.
Related: How to Treat an Mpox Rash
Who Is at Risk for Mpox?
Data and public messaging about the outbreak suggested that mpox disproportionally affects BIPOC and LGBTQ+ people—especially men who have sex with men. However, anyone can get infected by mpox.
“It’s crucial that we avoid stigmatizing language or perpetuating harmful stereotypes. Mpox transmission is linked to close physical contact, not any specific sexual orientation or gender identity,” said Brad Perkins, MD, the chief medical officer of medical biotechnology company Karius and a former chief strategy and innovation officer at the CDC. “An open, judgment-free dialogue that prioritizes facts over assumptions is vital for effective diagnosis, treatment, and prevention.”
While mpox spreads through skin-to-skin contact, it's not the only route of transmission, according to Tammy Lundstrom, MD, JD, senior vice president and chief medical officer at Trinity Health.
“It also spreads through contaminated materials, such as bedsheets or towels,” Lundstrom told Verywell. “A person with mpox is contagious from when symptoms develop until all the lesions heal. Early symptoms can be vague, like headache and fatigue, and there may be only a few lesions. People who think they may have been exposed and are not feeling well should avoid contact with others.”
Related: Mpox vs. Chickenpox: What Are the Differences?
Should You Get Vaccinated or Boosted?
Healthcare providers are focused on making sure that at-risk people can get the two-dose series of the Jynneos vaccine, the only vaccination currently available to protect against mpox. The CDC recommends that certain men, transgender individuals, or gender-diverse individuals who have sex with men should get the vaccine if, in the last six months, they have had:
One or more STIs
Sexual or intimate contact with a person who is at risk of mpox
Anonymous sexual or intimate contact or more than one sexual partner
Even though cases are increasing, experts say that booster doses of the vaccine are not recommended at this time if you’ve already received the shot at any point since its 2022 Food and Drug Administration (FDA) authorization.
On April 2, Jynneos manufacturer Bavarian Nordic announced that the vaccine is now commercially available in the U.S., opening up more options for patients and providers.
Brian Hujdich, the executive director of HealthHIV and the National Coalition for LGBTQ Health, told Verywell that stigma seems to be having less of an effect on vaccination rates for mpox compared to previous outbreaks of other conditions. He credits this response to the community’s past experiences with highly stigmatized conditions such as HIV/AIDS.
“I think that the perception that it primarily impacts gay and bisexual men persists,” said Hujdich. “But I’ve also seen, in a very encouraging way, that that hasn’t stopped the community overall in getting vaccinated and in showing an interest in their health care.”
However, Hujdich also pointed out that stigma still reduces the availability of routine medical care for the LGBTQ community.
“Both in the LGBTQ community and in BIPOC communities, there are challenges with housing and homelessness, and stigma and culturally incompetent care, that can directly and indirectly disconnect people from care, and especially from preventative care,” Hujdich said.
Related: What Does It Take To Be a Leader in LGBTQ+ Health Care?
Is Another Big Mpox Outbreak Coming?
The U.S. is not the only country affected by mpox right now. For example, the Democratic Republic of the Congo is currently experiencing an outbreak of a different strain of mpox.
The strain present in the U.S. appears to be milder. Noymer said that the strain of mpox in the U.S. is the same one that caused the outbreak in 2022, not the newer one in the Congo.
"It's important to be absolutely on top of the continuing mpox spread, but it's not something that people need to start hoarding toilet paper over," Noymer said.
Perkins said more research is still needed on the long-term impact and complications of mpox infection.
“Conditions like vision impairment, encephalitis, and scarring have been reported," Perkins added. "We need deeper research into characterizing and addressing these long-term sequelae.”
Read Next: How LGBTQ+ Individuals Can Find a Competent Healthcare Provider
What This Means For You
While mpox cases are rising, health experts aren’t overly worried. If you’re at risk of getting exposed to mpox, you should talk to your healthcare provider about getting vaccinated and other preventive steps you can take to protect yourself and others.
Read the original article on Verywell Health.

