I wonder if medical marijuana would have helped my late wife with multiple sclerosis
A lot has changed about how Americans view marijuana. A lot just since a day five years ago when my late wife’s doctor came down the hallway of her clinic in Southfield, waving papers at us.
Those changes include seeing marijuana shops spring up all over Michigan and across many other states. Billboards for legal weed sprung up, too. This year, the U.S. Drug Enforcement Administration is poised to pull marijuana from the category called Schedule I, where it was placed decades ago, for supposedly having no medical use and a high potential for abuse, listed alongside heroin and "ecstasy."
Yet, despite the changes, much of the marijuana coverage in the mainstream media and much of the research getting publicity continues to describe marijuana as a threat to health and a danger to society. Countless Americans still think marijuana is, bottom line, a bigger worry than alcohol. It’s time to dispute those outdated concerns — a myriad of myths, actually.
First, back to my memories. On a winter day in 2019, I sat in a doctor’s waiting room next to my late wife, who was soon to retire as a cop. My lady possessed two potent things along with her Glock: a mild case of multiple sclerosis rapidly turning virulent, and a career-long aversion to all street drugs, including marijuana. But when Dr. Tessie Jenkins brandished paperwork for getting a medical marijuana card, and said, “Eren, I really want you to try this,” my in-house security system — Sgt. Eren Stephens — surprised me. She said OK, she’d try this offbeat alternative to the FDA-approved pharmacy drugs she’d been taking.
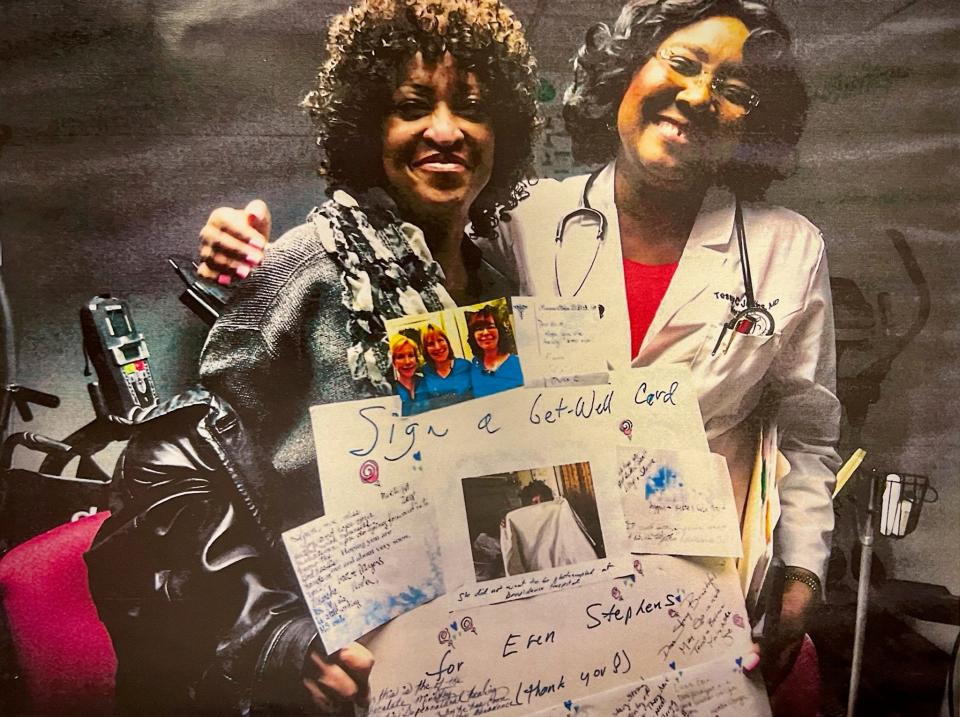
The pharmacy drugs had done little to stop her seizures, which were accelerating in frequency and severity. I learned how bad they’d gotten only after Eren’s death. I found a calendar book under her bed. She’d scrawled a record of her pain but kept it from me. On this winter day, though, as we basked in Dr. Jenkins’ smile and cheery words, I had hope for this new medicine that we’d grown up calling “weed” or “pot.”
These days, Jenkins is still a believer in medical marijuana, although with a difference. Now, she promotes the chemical component in marijuana that, in her practice, she says has shown significant health benefits — CBD. CBD is short for a chemical name that, at first blush, is all but unpronounceable: cannabidiol. Before turning to CBD, Jenkins had suggested medical marijuana to many of her patients. Now, she says she’s convinced that many of the benefits to her patients that medical marijuana provides "may just be coming from the CBD part of it.”
In 2018, the U.S. Food and Drug Administration approved CBD in the prescription drug Epidiolex, as an anti-seizure medication, although the FDA hesitated last year when asked to allow CBD in nutrition supplements. Still, Dr. Jenkins believes CBD in moderate amounts is safe for her patients and that the delay in giving it broader approval is similar to the stalling that surrounds the history of medical marijuana.
More: Waffle cone edibles, strawberry pre-rolls: Here's what new in Michigan's marijuana industry
“CBD has been studied quite extensively,” she says, demonstrating it to have anti-inflammatory and anti-anxiety effects. Jenkins prefers CBD to medical marijuana because CBD leaves out the main psychoactive substance in marijuana, called THC, “which makes people feel high; it causes your mood to change and my patients don’t need that,” Jenkins says. She’s a neurologist, in private practice since 2004, treating conditions of the brain, spinal cord and nerves.
Jenkins can cite other painful conditions that she has seen eased by CBD, which can be added to oils, creams and chewable sweet “gummies.” Those conditions include fibromyalgia, a mystifying condition of pain coursing throughout the body and accompanied by disrupted sleep, mood, and memory; neuropathy, the deadening of nerves usually starting in the feet and legs, often accompanied by stinging pains that doctors refer to as “pins and needles”; and many other ailments, from PTSD to dementia, as well as pain caused by numerous forms of cancer.
Jenkins sells three forms of CBD to her patients. One form has an oil base and a patient can place one or two drops under the tongue. A small bottle is $35. "That's mostly for pain but also for insomnia, PTSD and anxiety,” Jenkins told me on a recent visit to her office. She also sells a cream, telling patients to rub it on wherever they’re feeling pain, perhaps for back and neck pain caused by car accidents; and for the “burning feet” of diabetic neuropathy, when people with diabetes feel the intense pain of deteriorating nerves.
'If it works, buy it'
“I have people try it in the office and, if it works, they can buy it here” for $45 per container of cream, Jenkins said. One advantage of CBD in the cream form is that it lets patients avoid dosing their entire body with pain-relieving drugs that can leave them feeling drowsy and fatigued, unable to drive, work, or enjoy life, and which can damage the stomach lining with repeated use of high doses. A third form of CBD she sells is “gummies,” the sweetened chewable candies that taste like strawberries or raspberries: $40 for 100 pieces.

She found that CBD improves muscle elasticity, “so I give it to my MS patients,” she says. She goes on, “a lot of people are using CBD to help them sleep. And for epilepsy, it reduces seizures by 30%. There is a condition, Dravet’s Syndrome, that causes terrible things in children. CBD helps that.” Sure enough, according to a study in the March 14, 2018, issue of Neurology, a prominent medical journal: “Randomized controlled trials have suggested that an orally administered pharmaceutical formulation of purified CBD as an add-on to existing antiepileptic drugs has efficacy in treating convulsive seizures associated with Dravet syndrome and drop seizures associated with Lennox-Gastaut syndrome.”
Her prices and products are comparable to those at stores in metro Detroit, such as the Mother Earth Natural Health chain of CBD shops in Shelby and Chesterfield townships, Royal Oak and New Haven. Those shops don’t sell marijuana. Other shops that do sell marijuana, such as the Best Lyfe dispensary in Royal Oak, may also sell CBD products — from the “fruit chews” ($16 and $18 for packages of 10) to CBD-infused bath salts ($18) at Best Lyfe.
More: Michigan's cannabis industry turns 5 this year: What to expect
All carry a disclaimer: “These products are not for use by or sale to persons under the age of 18. The statements made regarding these products have not been evaluated by the Food and Drug Administration. The efficacy of these products has not been confirmed by FDA-approved research. … Please consult your healthcare practitioner about potential interactions or other possible complications before using any product. The Federal Food, Drug, and Cosmetic Act requires this notice.”
Jenkins, despite her focus on CBD, doesn’t condemn ordinary marijuana. She’s a firm believer in legalizing the drug. And to be fair, the THC component of marijuana has been shown in studies to possess its own array of therapeutic properties, particularly as a pain reliever. Some compounds sold for health combine CBD with THC, with THC giving an intoxicating effect. As for marijuana consumed in its raw form, Jenkins says it’s important to recognize that the drug, when made legal, tends to function as what might be called a reverse gateway drug: People switch to it from more dangerous substances, notably the addictive opioid pills that so frequently cause overdose deaths.

“In the states that approved legal marijuana, they’re finding a reduction in opioid use,” Jenkins says. Patients who were prescribed opioids tend to reduce or eliminate their use of opioids after they start using marijuana, according to numerous major studies. The most recent major findings, published in January 2023 in the eminent Journal of the American Medical Association, found that among 8,165 patients who were receiving opioid drugs for chronic pain, adding medical marijuana "was associated with prescription opioid dosage reduction (and) higher opioid dosages were associated with larger reductions … which may decrease patients’ risk of opioid overdose."
In Michigan, state law has approved the use of medical marijuana for 26 conditions, including seizures. Of course, after Michigan voters approved medical marijuana in 2008, they went on to approve legalizing the drug in 2018 for recreational use by those age 21 and over. Jenkins says she can’t be sure just how, and even whether, CBD will help a specific patient. She and the patient decide that by trial and error, just as medical doctors do with virtually all medicines they prescribe.
“I say to people who want to try CBD for seizures, ‘Don’t stop your regular medicine. Just try CBD along with whatever you’re taking.’ And then we see if they improve,” Jenkins says. She readily admits that she’s an outlier among her peers. Not many MDs recommend marijuana in any form. Most care for patients with warnings ringing in their heads from the American Medical Association, which continues to assert that legalized marijuana leads to more of everything from crime to car crashes to cancer — outdated myths that have been disproven by pioneering researchers, who studied marijuana before it was legalized, and by the sheer experience in countries and states where marijuana is legal and widely used.
For example, in states that legalized marijuana, naysayers said the incidence of traffic fatalities would go up. It some states, it did. In others, it went down. There's no clear connection, although repeated studies of test subjects who were placed on driving simulators after drinking alcohol on one occasion, and then tested again after smoking marijuana at another time, found that those who drank drove faster than usual and those who smoked drove slower. Jenkins says she’d prefer that her patients used marijuana, in any form, instead of alcohol.
“Alcohol is more dangerous,” she says. While allowing that modest amounts of red wine may protect the heart — may because research is mixed — Jenkins says alcohol is far more damaging than marijuana, to individuals and to society. For the chilling facts, check out a fact sheet titled “Marijuana Is Safer Than Alcohol: It’s time to treat it that way,” from the nonprofit Marijuana Policy Project (https://www.mpp.org/special/marijuana-is-safer/). Or skim a $15.50 paperback called "Marijuana is Safer; So Why are we Driving People to Drink?" (Chelsea Green Publishing).
The comparisons are shocking. Here’s one: Compare “there has never been a fatal marijuana overdose” to “the Centers for Disease Control attributes more than 1,600 U.S. deaths per year to alcohol poisoning.” Poisoning? That refers to people who drank themselves to death in just a single binge, which happens in college fraternity houses every year. “Poisoning” doesn’t include the far larger number of Americans who die from long-term conditions caused by alcohol, estimated by the CDC to be 178,000 Americans in a single recent year (2021, the most recent data available).
A fatal delay?
I’ll never know whether medical marijuana would’ve saved Eren’s life. We hit a delay in getting her medical marijuana card. Eren was denied on her first application. According to the denial letter from Lansing, the handwriting of the date next to her signature was deemed illegible by a state bureaucrat. Granted, it was a messy scrawl caused by her loss of muscle control.
On a second try, she practiced her cursive and her numbers, then worked very hard as I held a clipboard when she signed and dated the paperwork as neatly as she could — this, by someone who’d once studied calligraphy. Someone who, when we met, had the most beautiful signature I’d ever seen. Another month passed, and finally, on that second try, her official medical marijuana card arrived.
It got to us in a very busy week, a few days before Eren’s big retirement party at police headquarters. What a scene. She looked so good that day, surrounded by well-wishers, her table piled with plaques of commendation from city and county officials, and from her favorite charity — the Old Newsboys Goodfellows, whose gifts to the needy of Detroit had originally been delivered door-to-door by cops on their beats.
After the speeches and the friendly fuss made over her 31 years with the police department she loved, family members helped me get her into our car. Right then, we thought about visiting a marijuana shop — a dispensary. We knew of one nearby in Corktown. It was operated by Eren’s friend, who also had MS. But when we texted her, the friend said she was out of town. So we postponed our visit.
Three days later, I awoke to find that Eren was gone. She was just 60. I’ll always wonder if marijuana would’ve helped us. Maybe, it would’ve only postponed her last, fatal seizure. Maybe it would’ve prolonged her life and eased her final months or years. Maybe it wouldn’t have made any difference.
But it seems to be making a difference, in the form of CBD treatments, for the many patients of Dr. Jenkins. My favorite cop would be happy about that.
Contact Bill Laytner: blaitner@freepress.com
This article originally appeared on Detroit Free Press: CBD form of marijuana might've helped wife with multiple sclerosis

