Why There Aren't Enough Coronavirus Tests in the U.S.

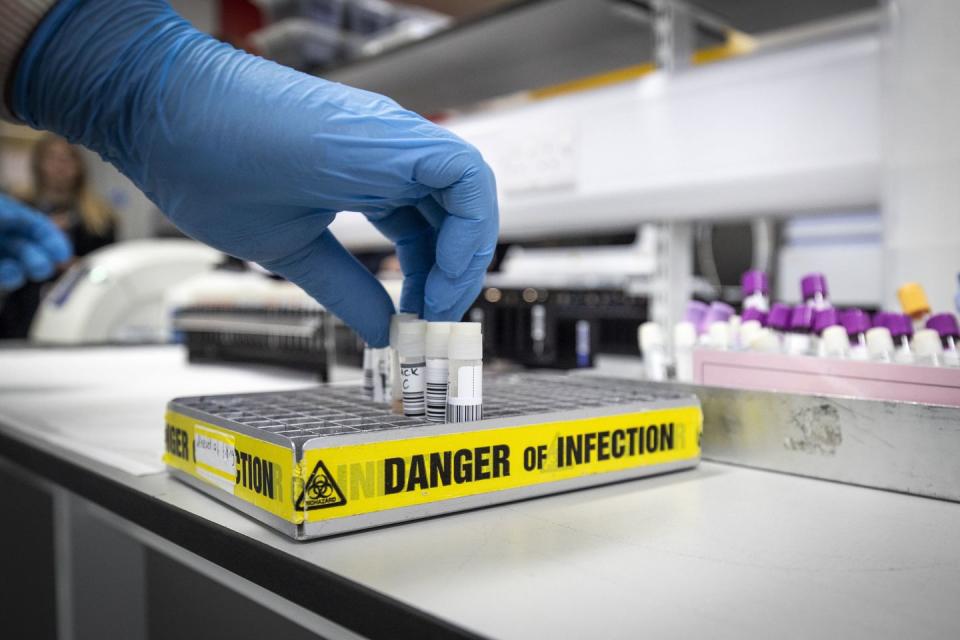
Above: A researcher works in a lab that is developing testing for the COVID-19 coronavirus at Hackensack Meridian Health Center for Discovery and Innovation on February 28, 2020 in Nutley, New Jersey. (Photo by Kena Betancur/Getty Images)
Although prior COVID-19 test kits had already been created, the U.S. Centers for Disease Control and Prevention (CDC) insisted on developing its own.
That led to time-consuming setbacks that have created a country-wide shortage of tests, leaving some sick people turned away.
In response, academic hospitals like the Cleveland Clinic have been developing supplemental tests to make them more widely available as the number of novel Coronavirus cases continues to rise in the U.S.
There's a massive shortage of COVID-19 (Coronavirus) test kits in the U.S., as cases continue to skyrocket in places like Seattle and New York City. This is largely due to the failure of the Centers for Disease Control and Prevention (CDC) to distribute the tests in a timely fashion.
But it didn't have to be this way. Back in January and February—when cases of the deadly disease began aggressively circulating outside of China—diagnostics already existed in places like Wuhan, where the pandemic began. Those tests followed World Health Organization (WHO) test guidelines, which the U.S. decided to eschew.
Instead, the CDC created its own in-depth diagnostics that could identify not only COVID-19, but a host of SARS-like coronaviruses. Then, disaster struck: When the CDC sent tests to labs during the first week of February, those labs discovered that while the kits did detect COVID-19, they also produced false positives when checking for other viruses. As the CDC went back to the drawing board to develop yet more tests, precious time ticked away.
"I think that we should have had testing more widely available about a month earlier," Dr. Carl Fichtenbaum, professor of clinical medicine at the University of Cincinnati's School of Medicine, tells Popular Mechanics. "That would have been more appropriate so that we could have identified people earlier on and used some of the mitigating strategies that we’re using now."
As the spread of Coronavirus continues to escalate in the U.S., private institutions like academic research hospitals are scrambling in a mad dash to come up with more test kits. And there is hope: the first human clinical trials for a possible vaccine have begun today.
How Does the COVID-19 Test Work?
Testing for COVID-19 comes in two primary forms: You'll either have your throat swabbed if you're in the U.S., or perhaps have your blood drawn if you're in another country, like China. The different approaches ultimately come down to how scientists have developed the lab tests.
In the U.S., the CDC's diagnostic tool relies on polymerase chain reaction testing (PCR), which detects genetic material found in the virus's RNA. Unlike in other methods, the virus doesn't have to be alive for its presence to be detected.
"We take parts of the virus and we [test] what’s called the conserved parts of the virus, parts that don’t change a lot," Dr. Fichtenbaum explains. "There are always mutations. We’re looking at the genetic code and we take a sequence of what we call primers, or things that will match up with that genetic code, and we put them through a series of steps where the primers will match the genetic code if [the virus] is present."
PCR testing is generally too advanced to be done at a hospital, and is more in the wheelhouse of clinical laboratory settings. There, researchers extract the sample's nucleic acid—one of the four bases found in DNA sequences—to study the virus genome. They can amplify portions of that genome through a special process called reverse transcription polymerase chain reaction. That way, scientists can compare the sample to SARS-CoV-2, the virus that causes the novel coronavirus.
SARS-CoV-2 has almost 30,000 nucleotides in total, which make up its DNA. The University of Washington School of Medicine's PCR test hones in on about 100 of those that are known to be unique to the virus.
The researchers are looking for two genes in particular, and if they find both, the test is considered positive. If they only find one, the test is inconclusive. However, the CDC notes, "it is possible the virus will not be detected" in the early stages of the viral infection.
In some cases, Dr. Fichtenbaum says, it's possible to quantify the number of copies of the viral gene present. It could be one, 10, or 10 million, he says, and the higher that amount is, the more contagious you may be, or the further along you may be in the illness.
Why Aren't There Enough Coronavirus Tests?

As of press time, the CDC has directly examined some 4,069 specimens in Atlanta, according to data produced on Monday afternoon, while public health laboratories across the country have tested another 18,644. Notably, some data after March 11 is still pending.
Regardless, with about 1,600 confirmed cases in the U.S., those figures suggest roughly one in 13 people tested have actually contracted the novel Coronavirus. Surely, if more tests were available, those numbers would be higher, Dr. Fichtenbaum says. Because of the CDC snafu and an initial muted reaction to the outbreak from President Trump's administration, we're about a month behind on the diagnostics front, he adds.
Piling onto other reasons, Dr. Karen C. Carroll—director of the Division of Medical Microbiology at Johns Hopkins University School of Medicine—believes that the test shortage is "complicated" by the fact that no one expected COVID-19 to spread so quickly in the U.S.
Not to mention, manufacturers are now low on supplies that academic labs, like hers, require to develop and distribute test kits, she tells Popular Mechanics.
During a Congressional hearing on Wednesday, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said the public health care system is failing to make tests available to people who may have contracted COVID-19.
"The idea of anybody getting [the test] easily the way people in other countries are doing it, we're not set up for that. Do I think we should be? Yes, but we're not," he said.
Updated to reflect #coronavirus testing capacity in hospital and clinical laboratories pic.twitter.com/WriCUMiyqS
— COVID-19 Test Capacity (@COVID2019tests) March 11, 2020
The silver lining: The CDC is now working in tandem with private labs to make more tests available. The concern then becomes how many tests these labs can actually perform each day. Experts estimate that most labs will have the capacity to complete about 100 tests per day, which just isn't good enough to contain COVID-19 at this point.
Who Is Actually Getting Tested?

Just because your doctor may have ordered you a COVID-19 test, that doesn't mean you'll actually receive one.
According to CDC guidelines, there are three general classes of patients who seek the diagnostic test, and it's up to the discretion of the health care systems to administer them. With limited supply, those are tough decisions. The classes are:
Hospitalized patients who have signs and symptoms compatible with COVID-19 in order to inform decisions related to infection control.
Other symptomatic individuals such as, older adults (age ≥ 65 years) and individuals with chronic medical conditions and/or an immunocompromised state that may put them at higher risk for poor outcomes (e.g., diabetes, heart disease, receiving immunosuppressive medications, chronic lung disease, chronic kidney disease).
Any persons including healthcare personnel, who within 14 days of symptom onset had close contact with a suspect or laboratory-confirmedCOVID-19 patient, or who have a history of travel from affected geographic areas within 14 days of their symptom onset.
Testing can be quite restrictive, and people who aren't in a high risk category, or who have traveled to a country where there are cases of COVID-19—but had no known exposure to the virus–are turned away.
"Once we relax the standards for testing so that we can test on anyone we think appropriate, and it’s not as complicated, we'll be able to reduce the spread," Dr. Fichtenbaum says.
Right now in Ohio, where Dr. Fichtenbaum is based, doctors must fill out a four-page form and conduct in-depth tracing of a patient's movements before they can administer a test, he says. Not only is it time-consuming, but it may result in the patient not receiving a test at all—and could have contracted the virus.
How do private labs develop new tests?

To expedite the availability of diagnostics, the U.S. Food and Drug Administration (FDA) announced in late February that academic hospital systems had the green light to develop their own test kits.
The move allows these institutions to rely on their own internal validation upfront, rather than wait on the time-consuming FDA approvals process before using the tests. While FDA approval is still ultimately required under this policy, once the hospitals themselves have determined the tests are accurate and safe, they can begin using them.
Dr. Carroll of Johns Hopkins says that her lab went live with their own test yesterday. "Now, we have 15 days to send [the FDA] our validation package," she says. Her lab can now use the test to check for COVID-19 in patients that come to the medical center, but a few more things must also happen in tandem to satisfy the FDA's requirements.
Once a private lab sends in their validation package, which includes data collected during the test development, the FDA may call back with questions about the kit or ask for clarification. If the labs get radio silence for a while, that's normal, according to Dr. Carroll, but eventually, they must be granted what is known as an Emergency Use Authorization.
Under section 564 of the Federal Food, Drug, and Cosmetic Act, the FDA Commissioner may allow unapproved medical products—like privately developed COVID-19 tests—to be used in an emergency for diagnosis, treatment or prevention when there are no better alternatives.
"I don’t know how quickly they will get back to laboratories, they haven’t told us that," Dr. Carroll says.
Labs must also have close communication with their state health department laboratory, which is essentially the top lab in the state, she added. The FDA is requiring private institutions to send their first five negative and first five positive testing results to their state lab to ensure uniformity and effectiveness.
"A public health laboratory monitors certain communicable diseases," Dr. Carroll explains. "Some even offer testing for the community, like STDs such as Gonorrhea."
More kits are on the way
Other hospitals across the U.S. are making strides in test development, too. In Washington, where the CDC's faulty tests stymied the progress of testing, potentially aiding the community spread seen there, the University of Washington Medical Center has developed a COVID-19 test based on WHO recommendations, unlike the CDC. The hospital system has the capacity to conduct about 1,000 tests per day, and is working to ramp that up to 4,000 or 5,000 daily tests.
The Cleveland Clinic's test, meanwhile, should only take about eight hours to turn around a positive or negative result and should be ready by the end of March.
In a statement provided Thursday to Popular Mechanics, the Cleveland Clinic says it will soon have the capabilities to conduct on-site testing. "We are in the process of validating our testing capabilities and will soon send out more information."
Moving forward, Dr. Fichtenbaum expects the FDA to soon approve what's known as multiplex testing, which will allow labs to run 96 tests at once, rather than work with one specimen at a time.
"They need to approve that at each lab and they’re slow," says Dr. Fichtenbaum. But he anticipates the FDA will give the all-clear in the next few days. Then, it's just a matter of manufacturing the tests, which should happen rapidly.
Sparking some hope, the first participant in a human clinical trial for a COVID-19 vaccine will receive the first experimental dose on Monday, an unnamed government official told the Associated Press.
The trial is taking place at the Kaiser Permanente Washington Health Research Institute in Seattle. Testing will eventually include 45 young, healthy volunteers who will each be given different doses of shots developed by the National Institutes of Health and Moderna, Inc., a Cambridge, Massachusetts-based drug discovery and development firm. The shots will not include the virus, itself, so there is no chance of the participants contracting the virus. The goal is simply to check for unexpected side effects. It will take at least 12 to 18 months for any potential vaccine to be validated and made available to the public, public health officials say.
In the meantime, community spread continues, despite self-quarantine measures, countless canceled events, and sweeping work-from-home policies. The number of positive cases is probably significantly higher than the data shows, says Dr. Fichtenbaum, which only worsens the contagion.
"I think that COVID-19 is probably more prevalent in our communities than we think," he says.
And the clinical microbiologists working tirelessly at the front lines in hospitals fully expect to meet testing demand. Dr. Heba Mostafa, assistant professor of pathology at Johns Hopkins University, tells Popular Mechanics that she expects to see testing ramp up and really meet demand over the course of the next four to eight weeks.
And Dr. Carroll says that the spirit of collaboration between academic medical centers has been refreshing. The University of Texas and the University of Washington have each helped out the Johns Hopkins effort, she says. They helped supply the genetic material necessary to complete their test's validation. Still, it's grueling.
"Our hospital is very happy that we went live yesterday, but of course now they’re interested in how many tests we can do," Carroll said with a laugh. "I sometimes feel that clinical microbiologists are the unsung heroes."
March 16, 2020: This story has been updated to reflect the beginning of human clinical trials for a possible Covid-19 vaccine. The number of Covid-19 tests distributed and taken in the U.S. has also been updated.
You Might Also Like

