Virtual doctor, virtual waiting room: New tech holds promise of speeding up ER wait times
A few steps inside the front door at Twin Oaks Memorial Hospital there's a new sign on the wall directing people to "Virtual Urgent Care."
What was once a conference room for hospital administration has been turned into a private space with large padded chairs and two iPad stations.
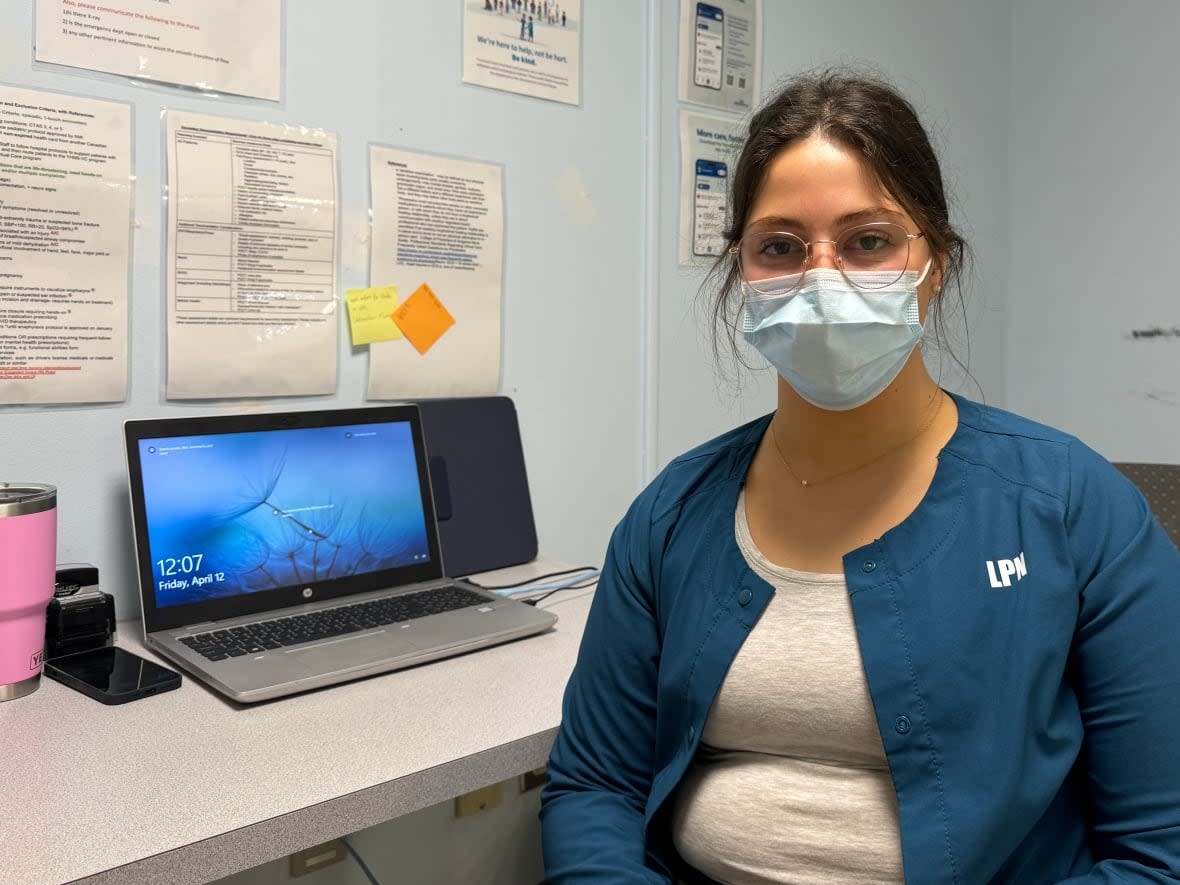
It's part of licensed practical nurse Samantha Langer's job to seat patients in the chair and connect them to a video call with an emergency-room doctor working far from the hospital in Musquodoboit Harbour, N.S.
"A lot of [patients] say pretty positive things," said Langer in a recent interview. "They're like, 'That's so cool, didn't know this even existed.' I get a lot of that."

As the Canadian health-care system struggles to deal with staffing shortages, many hospitals are increasingly seeing patients without access to primary care showing up in emergency rooms and facing long waits for relatively simple health issues.
To deal with the problem, some hospitals are turning to virtual technology, which they believe could move patients through the emergency room more efficiently.
The province didn't use virtual care much before the pandemic and "might have been quite late in the uptake even across Canada," said Tara Sampalli, a senior director at Nova Scotia Health whose work deals with science, innovation and health-systems planning.
But after the pandemic hit, the number of virtual visits jumped by 200 per cent, she said.
"All of us were surprised at how much we were able to [set] up in a rapid timeline."
100 visits a week so far
The iPad stations at Twin Oaks are one of nine up and running at hospitals around the province. The first started operating in November 2023 and the others started to come online in February.
The facilities are meant for "low-acuity" patients with problems such as coughs, colds, sprains, ear infections or urinary tract infections. Doctors who are working from home or even from another province are able to see patients, and prescribe next steps such as medication, tests or a referral for other hospital services. The doctors have to be licensed to practice in Nova Scotia.

The virtual-care sites are currently seeing about 100 visits per week, Sampalli said. She expects many emergency departments in Nova Scotia will have the capacity to offer a virtual urgent care station by June.
Three hospitals also have a different virtual program in which a nurse or paramedic stays in the consulting room with the patient to assist the remote doctor. It's for patients whose symptoms are more severe, but still within the scope of what remote medicine can handle. The eventual goal is to combine the two programs.
Program must be evaluated
Some front-line staff agree that virtual care in emergency rooms is the way to go.
Last fall, the province ran a contest to gather ideas from health-care workers, and many of the respondents wrote about the issue of patients coming to emergency rooms for routine matters such as prescription refills or blood work. Some suggested virtual care could solve that issue.
"I think placing a virtual care 'booth' in emergency rooms would improve the efficiency of patient care greatly," one submission said. "Something like a phone or computer station that would connect patients to a care provider that can handle minor ailments."
Since the program expanded in February, Sampalli said Nova Scotia Health has been calculating the costs and needs to analyze whether it's a net gain in terms of the financial investment and the amount of staff time it saves.
It is also too early to measure the effect of the program on wait times, she said, because it's being rolled out together with other measures like mobile clinics. But reports so far suggest the experience has been positive, she said.

The health-care ideas contest also received at least eight versions of a suggestion inspired by the restaurant industry.
"Give them a buzzer or send them a text or call when it's their turn," one person wrote. "Then patients can wait from the comfort of their own home where they'll be more comfortable, and waiting rooms will be less crowded."
Humber River Health, a large hospital in Toronto, has been reconsidering the issue of where patients should wait for treatment since 2019. Chief information officer Peter Bak said they even briefly considered the idea of using a buzzer, similar to one you might receive when waiting for a table at a restaurant.
"We thought, why do we do this to people? Why can't you sit at home or go to a Tim Hortons, or whatever it might be, and have a more relaxing time than sitting in a waiting room?"

Bak said the pandemic's arrival made the idea even more attractive.
In October, Humber River Health received a $1.5-million grant from a federal innovation fund to develop an online platform that would tell people coming to the emergency room to arrive immediately or give them a time slot to arrive, after asking a set of triage questions.
"Essentially we're just saying, 'stop waiting for us, don't come into the [emergency room] and wait. Wait at home,'" Bak said. "So it isn't changing the amount of time that you need to wait, but it's changing where you're waiting."
Bak said the hospital's clinical team has evaluated the platform and doesn't believe there's any increased risk to patients. He said it asks the same questions as standard telehealth services, and patients are encouraged to come in person if they feel their condition is getting worse.
Patient buy-in key
The platform will be piloted this summer, Bak said. He hopes it will allow the emergency department to better understand when patients are coming and what type of treatment they will need.
"I think the greatest measure is whether citizens adopt this and are comfortable and trust it," he said.
"The other measure of success is, if we are seeing the benefits back in the department itself: that we're seeing smoother flows, we're getting patients in and out faster."
If Humber River Health can make the technology work, its goal is to scale it up for other hospitals.
At Twin Oaks Memorial Hospital, so far the patients who are diverting from the emergency room into virtual urgent care have said they are open to receiving virtual treatments, according to Langer.
"Some people can still have a bit of a wait with virtual care, especially if there's a few patients that need to be seen before them. But so far it's been much quicker than the typical emergency department wait times," she said.
Do you have an experience with virtual emergency-room care in Nova Scotia to share? Write to us at cbcnsinvestigates@cbc.ca.
MORE TOP STORIES

