You’ve covered your copayment; now brace yourself for the ‘facility fee’
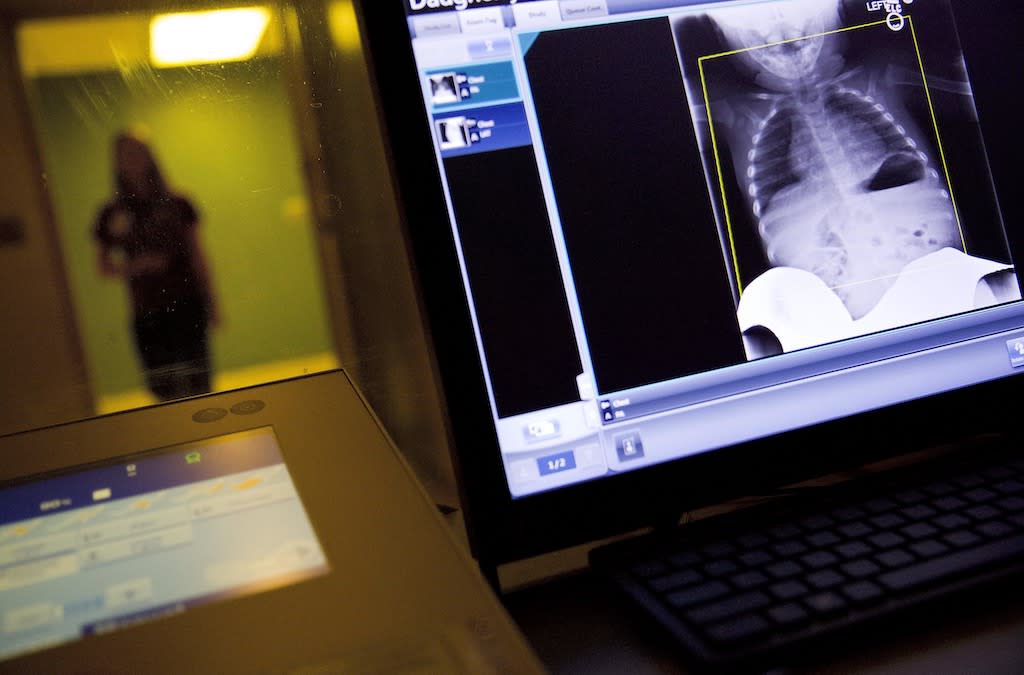
A radiology technician looks at a chest X-ray of a child suffering from flu symptoms at a medical center in Georgia. Hospitals increasingly are tacking on facility fees for routine services at the smaller clinics and outpatient centers that they own, even when those facilities aren’t anywhere near the hospital’s campus. David Goldman/The Associated Press
Even if you have health insurance, you might expect to be charged a copayment for some routine care, like office-based exams and consultations. But you probably don’t expect to receive a bill a few weeks later charging you an extra $100 or more.
That’s the situation an increasing number of state lawmakers are looking to change. In most states, a “hospital facility fee” can legally appear on your bill if your doctor is affiliated with a large hospital system — even if you never set foot on the hospital’s campus.
Traditionally, hospitals and health systems add facility fees to help cover the higher costs of operating a full-service, 24/7 hospital — which include expenses such as equipment, support staff, utilities, maintenance and security. They argue the fees help them provide critical services to everyone, regardless of their ability to pay.
But increasingly, hospitals are tacking on facility fees for routine services at the smaller clinics and outpatient centers they own, even when those facilities aren’t anywhere near the hospital’s campus. The fees can add anywhere from $15 to $100 or more to a medical bill. Patients have reported being charged out-of-hospital facility fees of $503 for a pediatric visit, $488 for an appointment to get ADHD medication, and $355 for steroid injections for arthritis.
Patients aren’t the only ones upset. Employers, aghast at the soaring costs of their employees’ health insurance, have banded together in states such as Indiana and Texas to push lawmakers to do something.
“Everything else at the provider’s office looks and feels the same,” said Maureen Hensley-Quinn, senior director of the coverage, cost and value team at the nonprofit National Academy for State Health Policy.
“But [patients] end up with a larger bill for a service they had previously gotten for a lesser amount because the hospital is now treating the provider office as a hospital outpatient department,” she said.
Hensley-Quinn said state lawmakers began relaying their constituents’ complaints to her organization about five years ago, and since then at least 15 states have taken action to address facility fees. Some, including Colorado, Connecticut and New York, have banned facility fees for certain outpatient services at non-hospital locations or for telehealth visits. Those states, as well as others, including Florida, Louisiana, Minnesota and Texas, now require hospitals to notify patients about facility fees ahead of time.
In the most recent legislative sessions, at least 16 bills were introduced in 10 states to address the fees, said Hensley-Quinn.
“It’s big states, small states, it’s very red states, very blue states,” she said. “Legislators across the country are raising these issues and asking questions about what increased consolidation means.”
More chains, fewer independents
A rise in fees and other patient costs springs from the growing consolidation of the American health care system, researchers and lawmakers say. Large hospital systems are gobbling up clinics, physician groups, and urgent care and imaging centers. Those facilities can then become outpatient departments of the hospitals.
A study published last year illustrates why hospital systems are motivated to make those moves: In the early 2000s, the federal government began cutting Medicare payments to doctors for noninvasive cardiac tests performed in a cardiologist’s office, but kept its payments flat or increased them for the same tests if they were performed in a hospital-based outpatient facility.
That dollar gap incentivized hospitals to acquire cardiology practices so that they could move cardiac tests to the outpatient facilities that could charge higher fees, researchers found.
More than a dozen states have passed facility fee laws just in the past few years, according to a recent report by the U.S. Public Interest Research Group, an advocacy nonprofit focused on consumer protection issues.
The efforts have been largely bipartisan. Indiana’s 2023 package of health care bills, which increased reporting requirements for hospitals charging facility fees, was authored by Republicans but passed with bipartisan support. That same year, Democratic lawmakers in Colorado passed a measure, with some Republican support, that prevents larger hospital systems from charging facility fees for preventive outpatient services.
Fees on the rise
Connecticut has the nation’s most robust facility fee laws. Last year, lawmakers expanded existing law to ban the fees for some routine outpatient services even if they’re performed on a hospital campus. The new law also beefed up state enforcement and created new reporting requirements for hospital systems.
“These fees are part of the increased cost of health care,” said Connecticut state Sen. Saud Anwar, a Democrat and a practicing physician who supported the new requirements. “Facility fees, depending on location, are a very fast-growing segment of that health care cost. We are looking for ways to control that.”
Hospital leaders say the fees help them cover overhead costs. That makes it possible for them “to maintain all the essential services they provide to their patients and communities, especially as Medicare and Medicaid continue to chronically underpay hospitals for the costs of delivering that care,” the American Hospital Association, a trade group, wrote in a statement to Stateline.
But prices for common outpatient services are significantly higher when they’re delivered in a hospital-owned outpatient department versus in a physician’s office or ambulatory surgery center, according to a 2023 analysis by Blue Health Intelligence, a division of the Blue Cross Blue Shield Association. For example, a mammogram performed in an office setting might bill insurance for $232, but in a hospital-owned outpatient department, facility fees bring the total to $357.50, according to the report.
These fees are part of the increased cost of health care. Facility fees … are a very fast-growing segment of that health care cost. We are looking for ways to control that.
– Connecticut state Sen. Saud Anwar, a Democrat and a practicing physician
And facility fees appear to be rising.
Last year, the Massachusetts Health Policy Commission found that the greatest increase in medical spending in Massachusetts’ commercial health care market was for hospital outpatient departments. Facility fees grew more than four times faster from 2019-2021 than physician/professional fees. The commission recommended lawmakers prohibit facility fees for common services such as lab tests, basic imaging and diagnostic services, as well as physician office visits.
In a 2020 study published in the journal Annals of Surgery, researchers found that facility fees for common outpatient procedures in the United States rose by 53% from 2011-2017, while physicians’ professional fees remained steady. The increases were primarily driven by facility fees and out-of-pocket expenses.
Back and forth
Not everyone’s convinced that banning or restricting facility fees will curb rising health care costs.
Last year, Maine lawmakers considered a bill that would have outlawed facility fees for services not located on hospital campuses. They ultimately chose instead to create a task force to study facility fees.
“The hospital association and other hospitals in the state came out pretty strongly against the bill, essentially saying facility fees are a billing mechanism to cover their costs — that all of their costs are essentially rolled up into their facility fees and they’d go bankrupt if they couldn’t bill for them,” said Lisa Nolan, director of legislative affairs at the Healthcare Purchaser Alliance of Maine, one of the stakeholder organizations involved with the task force.
Many rural hospitals and those that serve low-income communities are struggling financially, in part because of inadequate payments from insurers, according to the Center for Healthcare Quality and Payment Reform, a national policy organization.
More than 100 rural hospitals have closed nationwide in the past decade, and nearly 700 rural hospitals are at risk of closing in the near future. Some hospital leaders argue that removing the ability to charge facility fees could tip struggling hospitals into bankruptcy.
Maine’s task force recommended the legislature consider restricting facility fees for certain services, including telehealth. Yet many state lawmakers on the committee considering a new bill this year remained unconvinced. After some political wrangling, they passed a bill last month — now awaiting the governor’s signature — that requires health systems to notify patients about facility fees.
Nolan is skeptical that the laws banning facility fees would meaningfully reduce costs for consumers or insurance companies.
“Providers would find other ways to incorporate them into their bills,” she said. “There needs to be discussions about what are appropriate rates, how can providers be more efficient, and how can we reduce administrative costs for carriers and providers.
“Are some of those costs higher than they should be? That’s a different discussion than just wiping away facility fees.”
The post You’ve covered your copayment; now brace yourself for the ‘facility fee’ appeared first on Stateline.

