True impact of Covid on cancer patients revealed as excess deaths soar
The cost of the pandemic for cancer sufferers is starting to emerge, experts fear, as new figures show that hundreds more people than expected are dying each month in England from the disease.
Charities and health experts are calling for the Government to act, warning that missed diagnoses during lockdown may be a factor - and that the problem is being compounded by the current NHS crisis.
Since the beginning of September, there have been nearly 900 more deaths in people with cancer than would be expected at this time of year, the most recent breakdown of causes of death from the Office for Health Improvement and Disparities (OHID) shows.
There were nearly 230 extra deaths in the worst week.
Deaths involving heart complaints or diabetes have been on the increase since the spring, but it is only in recent weeks that the numbers dying from cancer have been above the five-year norm.
It comes as the Prime Minister has made addressing the crisis in the health service one of his top priorities, along with the cost of living and the surge in migrants crossing the Channel in small boats.
It is set to dominate the political agenda in the coming months, as winter pressures mount on the NHS.
Waiting lists are already at a record high, with a backlog of 7.1 million patients, and the numbers are set to keep rising until at least 2024.
On Sunday, Steve Barclay, the Health Secretary, admitted on BBC’s Sunday with Laura Kuenssberg that the health service was under “severe pressure”.
'That's not a challenge, that's a disaster isn't it?'#BBCLauraK shows Health Secretary Steve Barclay the statistics on A&E waiting times
Barclay says the NHS is 'under severe pressure' and funding was prioritised in the Autumn Statementhttps://t.co/5ephVBKlcb pic.twitter.com/zEvX5em8PB— BBC Politics (@BBCPolitics) November 20, 2022
He has vowed to cut red tape and centralised targets to give local hospitals more power, to ensure the extra £3.3 billion pledged for the NHS in the Autumn Statement last week is spent on frontline services rather than being soaked up by bureaucrats.
The Telegraph can reveal that half of NHS England staff face the sack under the plans.
Ministers want to slash the budget for the organisation’s 6,500 bureaucrats by as much as 50 per cent.
They favour a system modelled on the Tories’ school reforms where freedom for headteachers was backed by Ofsted inspections and exam league tables to hold them to account, leading to the UK rising nine places up the international education ratings.
The shake-up is expected to be spelled out in an NHS review commissioned by Chancellor Jeremy Hunt and Mr Barclay to find ways of giving hospitals greater autonomy, reducing “Stalinist” national targets and making them more accountable for how they perform and what they spend.
A Government source said: “Steve wants to cut out the pointless box-ticking and red tape so NHS staff can focus fully on caring for patients. He is determined to ensure every penny of investment goes into fixing the service rather than being squandered on ever-expanding layers of management.”
Urgent referrals hit new highs
Latest figures from the Office for National Statistics (ONS) show that there were 1,517 excess deaths in the week ending November 4, of which only 27 per cent (418) were due to Covid.
NHS data has shown that 38,000 fewer patients received a cancer diagnosis in England during 2020 - a 12 per cent drop from the previous year.
Analysis suggests that at least 22,000 fewer patients have undergone cancer treatment than would have been expected since the start of the pandemic.
The total number of urgent referrals for cancer has hit new highs this summer, with more than 255,000 cases in August - up from 190,369 in February 2020.
The total number of urgent referrals for cancer has also hit new highs this summer, with more than 255,000 cases in August - up from 190,369 in February 2020.
Professor Pat Price, chairman of Radiotherapy UK and co-founder of the #CatchUpWithCancer campaign, has urged Mr Barclay to intervene.
“The tragic reality is that the cancer backlog is the deadliest and most time-pressing of all and failure to tackle it will be measured in excess cancer deaths for years to come,” she said.
“There is a frustration to the point of despair amongst my clinical colleagues because it doesn’t need to be this way.”
Some of the worst cancer survival rates in Europe
Many patients failed to come forward during the pandemic for fear of being a burden on the NHS, while others were unable to access services as the health service turned its attention to Covid.
Dr Charles Levison, CEO of private GP DoctorCall said: “Excess cancer deaths were not immediately expected following delays throughout lockdown due to the nature of the disease, but clearly tens of thousands of people missing their cancer diagnosis was always going to result in excess death - I worry this is now starting to show.
“We’ve had several patients who delayed for a variety of reasons during lockdown. That led to a more advanced stage of cancer developing, with the associated complications. Worsened outcomes are inevitable and tragically that will result in fatalities.”
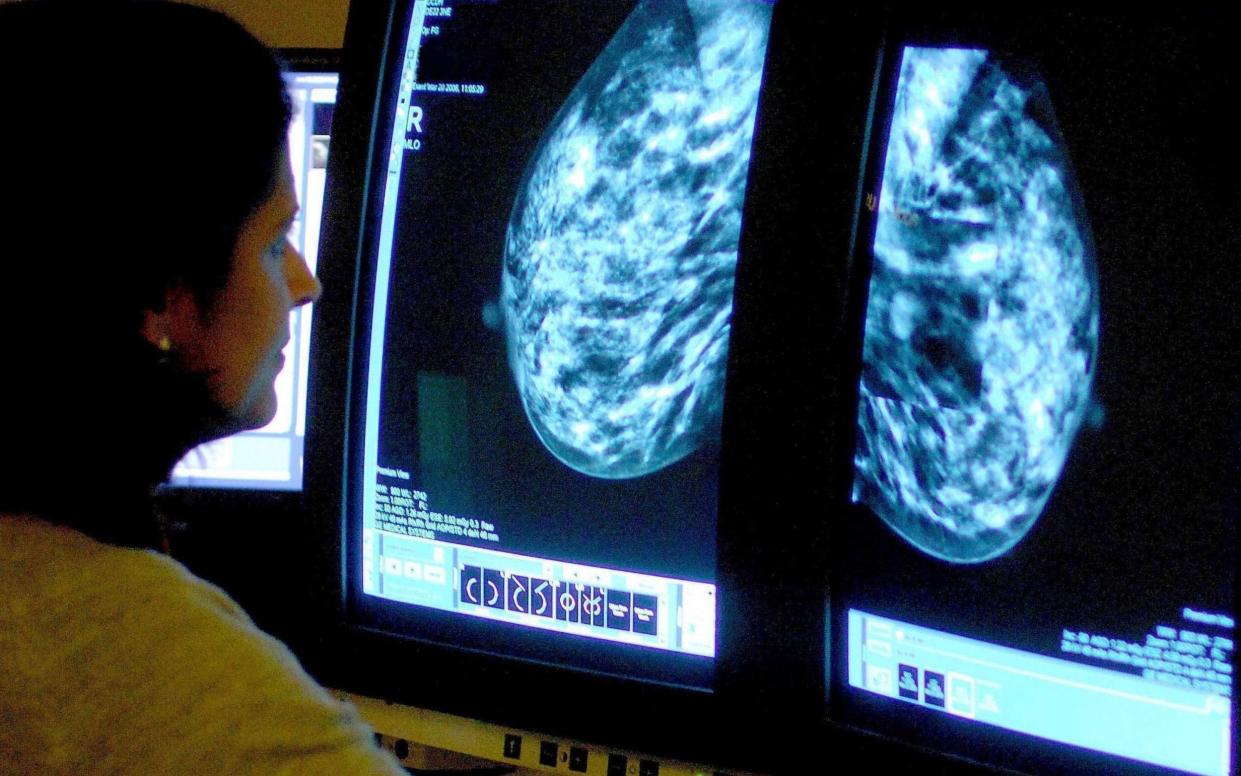
Melanie Sturtevant, associate director of Policy, Evidence and Influencing at Breast Cancer Now, warned that in 2020, over 8,200 fewer breast cancers were diagnosed in England compared to the previous year, (a 21 per cent decrease) as a result of Covid-19 disruption.
The charity has called on the Government to act.
“While it’s too early to know the long-term impact of the pandemic on breast cancer, we do know that the sooner breast cancer is diagnosed, the better the chances of treatment being successful and of lives potentially being saved,” she said.
“Thousands of people are currently living with undiagnosed breast cancer, making it critical the Government acknowledges the perilous situation impacting breast cancer diagnosis, and commits to addressing the underlying systemic issues, including urgently publishing a fully funded long-term workforce plan.”
The UK already has some of the worst cancer survival rates in Europe and Cancer Research UK has warned that Britain’s position among developed countries could get even worse.
‘Immeasurable more suffering is to come’
Dr Katrina Brown, stats manager at Cancer Research UK, said: “With cancer diagnosis and treatment performance having been so far off-target for so long – even before the pandemic – we are facing the possibility that cancer survival could go backwards.
“Screening effectively stopped during the pandemic, the number of people being referred for diagnostic tests dropped massively and a lot of tests and treatments for cancer were postponed.”
This week, GPs were told to fast-track cancer patients so they will receive a scan within four weeks rather than waiting 12 weeks to see a specialist before a referral.
But Karol Sikora, an oncologist, described the backlog of cancer treatment and missed diagnoses as a “total catastrophe”.
“Even our treatment targets, which are continually missed, are seen as woefully inadequate in neighbouring countries,” he said.
“Immeasurable more suffering is to come - where is the Government press conference on this?”
‘Stalinist centralism’
Before he became Chancellor, Mr Hunt said the NHS needed to ditch the “Stalinist centralism” that had given it more targets than any healthcare system in the world. GPs alone were tracked by a “whopping” 72 indicators which made them the “most micromanaged” on the planet.
“We should replace national targets with easily accessible data that allows everyone to compare performance. Care Quality Commission (CQC) Ofsted-style ratings work well.”
NHS England is already facing a 30 per cent to 40 per cent cut in its staff budget but ministers believe it could rise to 50 per cent under the review that will be led by Patricia Hewitt, former Labour health secretary.
Ministers believe the review by a Labour grandee, who also chairs the local integrated care system in Norfolk, will stymie any political criticism of the reforms.
Mr Barclay’s plans for reform of the health service include cutting central targets to free up hospitals to decide how they meet the needs of patients in their areas.
He told the BBC that the Department of Health had 50,000 employees in quangos and arms’ length bodies costing the taxpayer £2.8 billion. “That’s over 50,000 people that aren’t in directly patient-facing roles, so I think there’s opportunities in terms of merging those,” he said.
“It’s about looking at a local level how we design a healthcare system in a way that more empowers local leaders, better uses the population level data that we will have, and less diktat from the centre in a one-size-fits-all.
“That is one of the things those within the NHS tell me is causing a lot of noise, causing a lot of disruption and actually getting in the way of them delivering patient care… When I talk to Trust leaders, one of their frustrations is just the sheer amount of time they spend managing upwards.”
Mr Barclay has ordered all arms’ length bodies to publish “organograms” of their management structure to show what they do and how much they earn.
The first, by NHS England, showed it was employing 430 bureaucrats on over £100,000 each a year, of which a quarter were on at least £150,000. Forty-five earned more than the Prime Minister’s £164,000.
Major central targets such as ambulance waiting times and cancer treatment would remain, but others, such as the aim of admitting, transferring or discharging 95 per cent of patients coming into A&E within four hours - which has not been met since 2015 - could be scrapped.
Mr Barclay also said on Sunday that the Government had not abandoned the promised reforms of social care as he acknowledged the NHS was under “severe pressure”.
Matthew Taylor, chief executive of the NHS Confederation, the body which represents all areas of the health service, has said his organisation “absolutely supports” Mr Barclay’s proposals to devolve more power in the NHS.
He told Sophy Ridge on Sky News: “I strongly support the idea that we should try to devolve more power in the health service so that local health systems, working with partners like local government, can find solutions that work for them.
“Too often these national systems treat everywhere as if it’s the same, and places are very different.”
Mr Taylor added that “almost every hospital” in England, Wales and Northern Ireland “has got wards full of people who could go home, who should go home”, but there was a lack of social care staff to look after them.
He said the health service has an issue “about how we recruit, how we retain and how we motivate our staff”.

