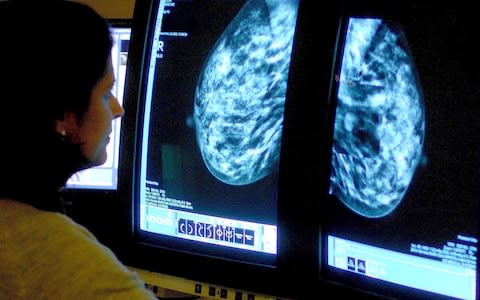
Thousands of breast cancer patients can safely avoid 'gruelling' chemotherapy, breakthrough trial finds

Thousands of breast cancer patients currently prescribed chemotherapy can safely avoid the “gruelling” treatment, according to a new trial hailed as the biggest advance in cancer practice for 20 years.
A long-term study of women with the most common form of the disease found less than a third should be put on the drugs, rather than the 50 per cent traditional figure.
The trial found that for a significant proportion of the patients diagnosed at an early stage, their survival chances were just as good if they took only oral hormone medication, which comes with far fewer risks and side-effects.
The results have been welcomed as “fantastic news” by cancer charities, while leading oncologists said they should “transform care immediately”.
Dr Alistair Ring, a Consultant in Medical Oncology at the Royal Marsden hospital in London: said: “On Monday in the clinic, I will offer less chemotherapy that will not be of benefit to patients, and that is very reassuring.”
Scientist at the Montefiore Medical Centre in New York studied more than 10,200 women with hormone receptor-positive, HER2-negative, axillary node-negative breast cancer, a type which affects around 23,000 British women a year.
It’s fantastic news that this landmark study could now enable thousands more breast cancer patients over 50 to be safely spared gruelling chemotherapy
Baroness Delyth Morgan
Biopsies were taken from their tumours and subjected to the Oncotype DX genetic test, available on the NHS, which gives patients a risk score of the disease returning after surgery, based on examining 21 genes.
The women then received either chemotherapy with hormone drugs, or hormone drugs alone.
After a nine-year follow-up, the researchers noted that patients who had been given an “intermediate” risk score had an almost identical chance of surviving - 93 per cent - regardless of which regimens they were on.
About | Breast cancer
Under current NHS practice, many UK women with this score are currently put on chemotherapy.
Experts calculate that, thanks to the results of the TAILORx trial, up to 5,000 British patients a year can now be spared the treatment.
Baroness Delyth Morgan, Chief Executive of Breast Cancer Now, said: “It’s fantastic news that this landmark study could now enable thousands more breast cancer patients over 50 to be safely spared gruelling chemotherapy.
“This is another significant step towards personalised breast cancer treatment and we hope these practice-changing findings will now help refine our use of chemotherapy on the NHS.”
Breast cancer survival has roughly doubled in the UK over the past four decades, with chemotherapy a “cornerstone” of treatment.
The side effects can be notoriously severe, including nausea, vomiting, hair loss, fatigue and early menopause in the short term, with a higher long-term risk of developing heart failure and even leukemia.
However, Dr Ring said that better understanding of the risk scores provided by gene assay tests such as Oncotype DX marked a “step-change” in the targeted use of chemotherapy.
He said the new study was equal in significance to the advance of cancer treatment to the arrival of Herceptin in 1998, which gave hope to the roughly 20 per cent of breast cancer patients with the HER2-positive form.
Around 20,000 British women have undergone the Oncotype DX gene test since its development in 2013.
In January, the National Institute of Health Care Excellence (Nice), which sets clinical guidelines, caused alarm when it said it would be reviewing the test’s use on the NHS, however the body is now expected to recommend its continued use.
Five cancer red flags to never ignore
“Before TAILORx, there was uncertainty about the best treatment for women with a mid-range score of 11-25 on the Oncotype DX Breast Recurrence Score test,” said Dr Joseph Sparano, who led the US Government-funded research.
“The trial was designed to address this question, and provides a very definitive answer.
“Any woman with early-stage breast cancer 75 years or younger should have the test and discuss the results of TAILORx with her doctor to guide her decision regarding chemotherapy after surgery to prevent recurrence.”
Slashing the number of women needing chemotherapy would take more than £13 million off NHS bills and could also improve waiting times.
A course of chemotherapy typically costs the NHS £4,500, whereas the list price of the Oncotype DX test is £2,500 each, however the NHS says it pays less thanks to a confidential deal with the manufacturer, Genomic Health.
Dr Harold Burstein, a leading Asco oncologist, said the new data had the capacity to “transform care immediately, and for the better”.
“Practically speaking, this means that thousands of women will be able to avoid chemotherapy, with all of its side effects, while still achieving excellent long-term outcomes,” he said.

