New therapy could help treat skin infections without turning them into superbugs
With concerns about the rise of so-called "superbugs" at an all-time high, scientists are on a mission to find better ways to tackle infections. And a new study, published last week in the journal PLOS ONE, claims to have done just that.
The research describes a new strategy that aims to tackle skin infections — which can be particularly dangerous in hospital patients and the elderly — without creating antibiotic-resistant bacteria in the process.
SEE ALSO: 3D-Printed Bacteria May Unlock Secrets of Disease
The treatment works by making it harder for bacteria to stick to human cells and therefore easier to wash away.
Most importantly, the treatment has a low risk of contributing to the rise of antibiotic-resistant bacteria. And according to scientists, developing such treatments is critically important.
The "superbug" problem
Experts agree that antibiotic-resistant bacteria are a growing problem, and are largely the result of the excessive use of antibiotics in recent decades.
Antibiotics are generally designed to treat infections by killing bacteria en masse. The problem is that in any given colony of bacteria, a few individuals may have special genes that render them resistant to the antibiotics. So when the rest of the population dies off, these individuals remain and can pass on their genes, giving rise to whole strains of resistant bacteria.
Often, such bacteria can still be treated with more aggressive drugs. But some types of antibiotic-resistant bacteria may be more challenging and sometimes not treatable at all, according to Paul Fey, a professor and Staph expert at the University of Nebraska Medical Center.
Just a few months ago, in fact, researchers announced the first case of a patient in the U.S. carrying bacteria resistant to even the most aggressive "last-resort" antibiotics. The incident has sparked concern among health officials that the nation could eventually witness the rise of multi-drug resistant superbugs, impossible to treat with existing antibiotics.
A new therapy for skin infections
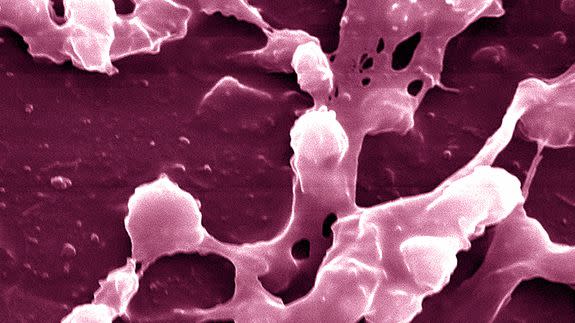
The new study focuses on a type of bacteria called Staphylococcus aureus, or "Staph" — one of the leading causes of skin and wound infections. Staph can be especially dangerous in hospital patients, the elderly and other people whose immune systems may be compromised and less capable of tackling infections on their own.
A type of antibiotic-resistant Staph, commonly known as MRSA, is especially dangerous. The CDC estimates that more than 80,000 invasive MRSA infections occurred nationwide in 2011. MRSA infections are more difficult to treat than regular Staph infections, and when severe enough, they can move from the skin into the bloodstream and even become fatal.
Staph bacteria use certain mechanisms to stick to human skin cells and launch infections. One way they do this is by interacting with special types of proteins in skin cells called "tetraspanins." These proteins are involved in all kinds of important cell functions, but they also have properties that make them “sticky” to foreign cells and molecules — meaning bacteria can exploit them as a way to infect human cells.
"You can think of them as like a patch of velcro sticking out from the surface of the skin cells," said Sheila MacNeil, a professor of tissue engineering at the University of Sheffield and one of the new study’s authors, in an interview with Mashable.
In the new study, the researchers synthetically created a series of peptides — special molecules composed of a chain of amino acids — that they hoped would make it more difficult for bacteria to cling to these spots.
The researchers tested their peptides on several types of skin cells in the laboratory, as well as a special 3D, lab-created human skin model to test the peptides on.
The researchers found that their peptides worked best in cells called keratinocytes — the body’s outermost layer of skin cells and first line of defense against infections — where they were able to reduce the bacterial burden by about 50 percent. They received similar results in their tests on the 3D skin model.
The researchers can’t yet say for sure exactly how the peptides are causing this effect, but they know the treatment somehow reduces the "stickiness" of the tetraspanins.
Importantly, the treatment worked on antibiotic-resistant Staph strains — and it also showed no signs of killing the bacteria, meaning it has a low likelihood of contributing to the rise of new antibiotic-resistant strains. The treatment also didn’t seem to have any adverse effects on the human cells.
That said, this study suggests that the treatment only helps to remove about half the bacteria from skin cells. According to MacNeil, the researchers hope the therapy can reduce bacterial burdens just enough to make it easier for the patient’s immune system to start tackling the infection.
The future of antibiotics
To be clear, the new study only describes the method’s effects in a laboratory setting. But the researchers are planning to conduct additional tests over the next few years and hope the treatment can be tested in clinical trials (meaning with real humans) within three to five years.
If successful, the researchers hope the peptides could be placed in creams, gels or sprays that could then be applied to wounds. Such treatments would likely be most appropriate in high-risk populations, such as hospital patients or people undergoing surgery, said Fey, the University of Nebraska professor (who was not involved in the new study).
It's certainly not the only strategy that’s been explored when it comes to the fight against superbugs.
"There are a lot of pharmaceutical companies looking at vaccines against Staphylococcus aureus," Fey pointed out. And other studies have explored therapies aimed at boosting patients’ immune systems to help them tackle infections with less help from antibiotics.
The new research only adds to this arsenal of strategies.
"[In the future] I think there will be a lot of development of therapies that tackle bacteria that work alongside the patient’s immune system," MacNeil said. "We still need antibiotics, but we need to use them a lot less and only use them when we absolutely need."
