How to Spot a Meningitis Rash (And What to Do Next)
Medically reviewed by Marisa Garshick, MD
Meningitis refers to an infection of the meninges, the membranes that surround and protect the spinal cord and brain. It can be caused by a viral illness or certain bacteria. Bacterial meningitis is a life-threatening emergency.
When bacterial meningitis leads to sepsis (a blood infection), also known as meningococcal septicemia or meningococcemia, it can cause a meningitis rash on the skin. A meningitis rash typically looks like pinpricks or bruises, which may be red or dark purple. This rash doesn’t fade when you press a glass against it.
In this article, we’ll review everything you need to know about the meningitis rash, including what it looks like, why it happens, and how to conduct “the glass test.”

janiecbros / Getty Images
Understanding Meningitis Rash
If Neisseria meningitidis bacteria, which causes meningitis, invade the body and bloodstream, they can cause an infection that damages internal organs and blood vessels. This damage causes the rash often associated with severe cases of meningitis. This “rash” is broken blood vessels that are leaking under the skin, which makes it look different from many other, more typical rashes.
What Does a Meningitis Rash Look Like?
Meningitis rashes can look very different from person to person, depending on their skin tone, how far their disease has progressed, and many other factors. Not all cases of meningitis lead to a rash, but it is a sign that you or your child needs immediate medical attention.
A meningitis rash often begins as a “petechial rash,” meaning it causes purple or red pinprick-like spots on the skin. Later, it may become a “purpuric rash,” which means it looks like large blotchy bruises, which may be red, purple, or brown.
These spots can appear anywhere on the body, but they are especially common on the legs, feet, and pelvic area. If the rash progresses, it can extend to areas of the face, such as the eyes, nose, and lips.
Meningitis rashes are harder to see on darker skin. You may be able to spot the pinpricks or blotches on lighter parts of the body, such as the:
Whites of the eyes
Inner eyelids
Soles of the feet
Palms
Stomach
Roof of the mouth
At first, a meningitis rash is often blanching, which means it turns white or lighter when you apply pressure to the area. If the bacteria continues to spread and cause serious damage, it may become non-blanching, meaning it does not go away when you press it.
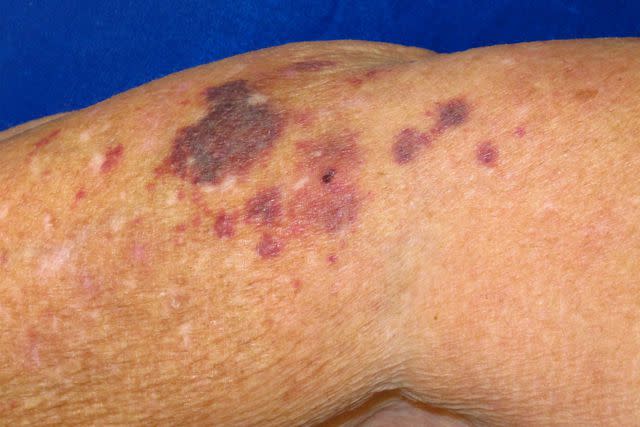
Reproduced with permission from © DermNet and © Te Whatu Ora dermnetnz.org 2023.

Reproduced with permission from © DermNet dermnetnz.org 2023.
Other Meningitis Symptoms
In addition to a distinctive rash, people may experience the following symptoms of meningitis, including:
Fever
Other skin-related symptoms, such as skin discoloration or mottled skin
Joint pain
Muscle pain
Cold extremities
Nausea
Disorientation
Headache
Stiff neck
Photosensitivity (light sensitivity)
Lethargy (lack of energy)
Shortness of breath
Fatigue
Diarrhea
Chills
Symptoms in Infants and Children
Babies and young children may have different signs and symptoms of meningitis, such as:
Irritability
Excessive, high-pitched crying
Floppiness or stiffness
Sleepiness
Lack of responsiveness
Lack of appetite
A bulging fontanelle (soft spot) at the top of the head
Vomiting
Slower reflexes
The Glass Test
“The glass test,” also known as the “tumbler test,” is often used to determine whether or not a skin rash is caused by meningitis. It involves pressing a glass against the affected area of the skin and seeing if the rash goes away. If it doesn’t, you or your child may have a non-blanching rash due to meningitis. It is a sign that you or your loved one needs emergency medical care.
How a Meningitis Rash Is Diagnosed
It’s not always easy to diagnose meningitis right away. If you have a meningitis rash or any other potential symptoms of meningococcal disease, your healthcare provider will typically be able to diagnose your condition through tests, such as:
Serum (blood) tests
Cerebrospinal fluid samples
Cultures for Neisseria meningitidis bacteria
Because meningitis is serious and even fatal, your healthcare provider must start treating you immediately. Meningitis can be treated with:
Antibiotics to treat bacterial infections
Anti-viral medications to lessen the length and severity of your illness (if you have viral meningitis)
Breathing support, such as oxygen therapy, if you have trouble breathing
Surgery and/or wound care if your skin has been extensively affected
Who’s at Risk for Meningitis?
There are several risk factors that may put someone at a higher risk for developing meningitis, including:
Age, including being less than 1 year old, between the ages of 16 and 23, or over 65
Having certain medical conditions, such as asplenia (not having a spleen), spleen-related disorders, complement component deficiencies, or the human immunodeficiency virus (HIV)
Taking certain medications, such as Soliris (eculizumab) or Ultomiris (ravulizumab)
Traveling regularly to certain parts of sub-Saharan Africa
Having a job that requires you to work with meningococcal bacteria
Living in a communal setting, such as a college dorm, a shelter, or a military barrack
Long-Term Meningitis Complications
The most common long-term complications of meningitis may include hearing loss or neurological damage, including brain damage and other problems with the nervous system. In severe cases, meningitis can also lead to limb loss. If your meningitis rash spreads and blood vessel damage is extensive, oxygen may fail to travel to your extremities (legs, feet, arms, and hands) effectively. This could lead to tissue death and require the amputation of one or more limbs.
Other potential complications of meningitis may include:
Vision loss
Arthritis
Kidney problems
Seizures
In children, problems with learning and behavior
Problems with memory and concentration
Problems with coordination and balance
Is Meningitis Contagious?
While meningococcal bacteria can be spread through saliva, meningitis isn’t usually as contagious as other viral illnesses. You can catch meningitis through prolonged close contact with someone who has meningitis, such as:
Sexual contact
Sharing personal and/or household items with someone regularly
Giving and receiving medical treatment
If one of your close contacts, such as a sexual partner, family member, or roommate, has been diagnosed with meningitis, your healthcare provider may recommend that you take antibiotics even if you aren’t showing any symptoms.
Vaccinations are also available to prevent some types of bacterial meningitis. The haemophilus influenzae type B (Hib) vaccine is given to infants and children, and the pneumococcal and meningococcal vaccines can be administered to both children and adults.
What Other Rashes Look Like Meningitis?
There are a few other rashes that can be confused with meningitis, such as:
Other petechial and purpural rashes: Petechiae and purpura are always caused by bleeding under the skin and in the mucous membranes. Petechiae are tiny, measuring less than 4 millimeters (mm) in diameter; purpura may measure up to 10 mm across. Meningococcemia is not the only cause of these skin conditions. They can also be related to viral illnesses like COVID-19, other blood disorders, the effects of aging, taking certain medications, and more.
Vasculitis: Vasculitis, which refers to the inflammation of the blood vessels, can cause a type of purpural rash known as Henoch-Schönlein purpura.
Hives: Hives are small, raised bumps that often appear in clusters across the skin. Allergic reactions often cause them, but viral illnesses can also cause them. Unlike petechial and purpural rashes, hives are typically itchy and swollen.
Even if you aren’t sure if your skin condition is caused by meningitis, it’s best to seek medical care immediately.
When to Contact a Healthcare Provider
Early treatment is key when it comes to preventing serious and even fatal medical complications of meningitis. If you or your child develops a skin condition that looks like a meningitis rash, seek emergency medical help. Call 911 or go to the hospital right away.
It’s important to remember that not everyone with meningitis will develop a rash. Some people may not develop one, while others might have a milder version or one that looks atypical. Even if you don’t have a rash, it’s crucial that you get immediate medical assistance if you think you may have meningitis.
Summary
A meningitis rash is caused by meningitis, which occurs when the meninges surrounding the brain and spinal cord get infected with meningococcal bacteria.
The rash is distinctive, often like clusters of pinpricks or large bruises. It’s typically a non-blanching rash, meaning that it maintains its appearance even when you press something against it. However, it can present in many different ways.
Meningitis is a life-threatening condition. Call 911 or go to the emergency room if you or a loved one develops a meningitis rash or any other symptoms of meningococcal disease.
Read the original article on Verywell Health.

