Republican health bill stirs fear in opioid-wracked West Virginia
By Chris Kenning
(Reuters) - Debra Bright said she battled for years with mental illness and addiction to pain pills and other drugs that were all too easy to find where she lives in West Virginia, one of the states hardest hit by the country's opiate epidemic.
Now Bright, 42, fears the bill passed on Thursday by the Republican-controlled House of Representatives to repeal Obamacare will roll back the Medicaid insurance coverage that has enabled her to get drug and mental health treatments she would not have been able to afford otherwise.
"There is so much addiction here, if they pull the medical cards – this place, it's done," said the former waitress and mother of four, referring to the cards held my Medicaid recipients and possible reductions in coverage under the legislation, supported by President Donald Trump.
"I hope the president really considers what he's doing here," said Bright, who lives in the western part of the state.
She is not alone in her fears. In states like West Virginia, which voted overwhelmingly for Trump in November's election, the House bill has stirred deep concerns over its potential effect on drug and mental health programs, in part because it gives states discretion over such spending.
Supporters of the bill, including House Speaker Paul Ryan, have said those concerns are overblown.
Under the Affordable Care Act, or Obamacare, a 2010 law that enabled 20 million more Americans to get health insurance, more than 30 states, including West Virginia, opted to expand eligibility for Medicare. That added 11 million people to the rolls of the insurance program for the poor.
Obamacare required Medicaid and individual private insurance plans to cover "essential health benefits" including substance abuse and mental healthcare, enabling more people who formerly did not qualify for services such as residential treatment and mental health therapy to pay for them.
That was particularly helpful in West Virginia, which has the country's highest opioid overdose death rate and the highest percentage of adults aged 19 to 64 on Medicaid at 26 percent.
The American Health Care Act passed on Thursday would roll back the Medicaid expansion and slash the program’s funding. By 2020, it would allow states to decide whether to include mental health and substance abuse recovery benefits in Medicaid and individual-market plans. The Senate must still approve the legislation.
The National Council for Behavioral Health in Washington, D.C., said the House bill would eliminate $880 billion from Medicaid over 10 years and leave many states little choice but to reduce Medicaid rolls or cut services such as mental health or substance abuse programs. It said that nationally, 29 percent of those on Medicaid have some form of substance abuse or mental illness.
Opioids, including pain pills and heroin, killed more than 33,000 people in the United States in 2015, more than any year on record, according to the Centers for Disease Control and Prevention. It estimated in 2016 that the cost of opioid abuse in healthcare, drug treatment, criminal justice and lost productivity was $78 billion a year.
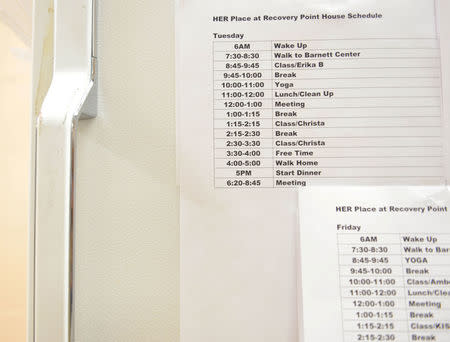
"We're experiencing a huge problem, but we're seeing a lot of people get well because they're able to access services," said Matt Boggs, executive director of Recovery Point West Virginia, which runs four residential treatment centers where nearly all clients are enrolled in Medicaid.
Paul Howard, director of health policy at the conservative Manhattan Institute, said states have ways of providing services outside Medicaid, arguing that Medicaid costs need to be contained. He said if necessary Congress could set aside funds to deal with crises such as opioid abuse.
Trump has said the Republican proposal would give states more flexibility in how Medicaid dollars are spent.
But health providers in states with some of the highest rates of opioid overdoses have said Medicaid expansion has been a boon for the fight against the U.S. drug crisis.
More than 1.8 million people got treatment for mental health and substance abuse disorders under the Medicaid expansion and on individual plans provided under Obamacare, according to Richard Frank, a Harvard Medical School healthcare economist, amounting to $5.5 billion of services.
In Ohio, Medicaid now pays for half of all medical-assisted drug treatment, according to the National Council for Behavioral Health. In Kentucky, that figure is 44 percent. States have not said how they might cope with reductions in Medicaid funding or if they would alter covered benefits.
In West Virginia, Bright said she has been drug-free for more than 100 days. She hopes she does not lose the benefits that enabled her to get help.
"If they make it so only people who have money gets help, it's going to be bad," she said.
(Reporting by Chris Kenning; Editing by Ben Klayman, Toni Reinhold)
Related Video: 9 Million Painkillers Shipped to Tiny West Virginia Town
For more news videos visit Yahoo View, available on iOS and Android.