Pigment Dispersion Syndrome
Medically reviewed by Johnstone M. Kim, MDMedically reviewed by Johnstone M. Kim, MD
Pigment dispersion syndrome is an eye disease that occurs when pigment granules are released from the back of your iris (the colored part of the eye). The loose fragments float around in the aqueous humor (the clear fluid that fills the front part of your eye).
These flakes can clog drainage canals and increase intraocular pressure (pressure in your eye). High intraocular pressure (ocular hypertension) can damage your optic nerve. This nerve transmits visual images from your eye to your brain.
Pigment dispersion syndrome is often underdiagnosed because it mostly affects people in their 20s and 30s, ages when eye problems are not common. It can exist without symptoms and is typically found during a routine eye exam.
Treatment involves decreasing eye pressure with drugs, laser treatment, or surgery. Early diagnosis and proper treatment can yield positive results.
This article describes pigment dispersion syndrome's causes, risk factors, and symptoms. It also explains the diagnosis, treatments, and outlook for this problem.
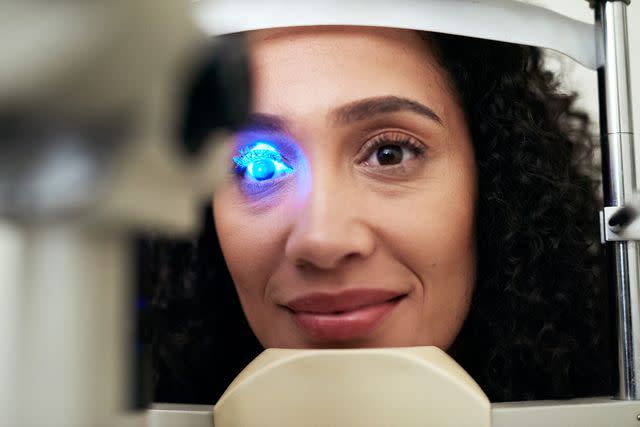
LaylaBird / Getty Images
What Causes Pigment Dispersion Syndrome?
Though the exact causes of pigment dispersion syndrome are unknown, certain factors can contribute to the development of this eye disorder:
Concave iris: People with this condition typically have an abnormal iris. The iris is concave, which results in the back of the iris rubbing against fibers from your eye lens.
Genetic predisposition: There is evidence that pigment dispersion syndrome involves a genetic predisposition because the disease tends to run in families. However, the exact genes linked with this condition are unknown.
Age: Pigment dispersion syndrome typically affects people between the ages of 20 and 40, with early adults diagnosed the most often. This disease occurs less often with age, which may be related to the physical changes in your eye that occur with age.
High myopia (severe nearsightedness): Having high myopia may increase your risk of having pigment dispersion syndrome. The structural changes that occur with high myopia, such as a more concave shape to your iris, can increase the likelihood of your iris rubbing against your lens or other eye structures.
Learn More: Overview of the Iris of the Eye
Risk Factors for Pigment Dispersion Syndrome
Though pigment dispersion syndrome can affect anyone, people with one or more of the following risk factors are more likely to get this disease:
Assigned male at birth
White race
Nearsightedness
Age 20 to 40 years
Family history of pigmentary dispersion syndrome or pigmentary glaucoma
Pigment Dispersion Syndrome Symptoms
Pigment dispersion syndrome symptoms do not occur in all cases. It is possible to have the condition and not know it until it is discovered during an eye exam.
Symptoms of pigment dispersion syndrome are linked with an increase in eye pressure. You may notice these changes more often after exercise. Episodes of symptoms may occur as your optic nerve becomes more damaged:
Hazy or cloudy vision
Halo effects when looking at bright lights
Eye pain, often described as a dull ache or pressure sensation
Swelling of your cornea (the clear dome of tissue at the front of your eye)
Eye floaters (spots in your visual field)
Learn More: Symptoms of Glaucoma
How Pigment Dispersion Syndrome Is Diagnosed
Because this condition is often asymptomatic, pigment dispersion syndrome is often diagnosed during a routine eye exam. From a clinical perspective, the disease is associated with a finding of Krukenberg's spindle, a narrow or rounded oval of brown pigment on the inner surface of your cornea.
Depending on your symptoms, a comprehensive eye exam can include the following tests that assess your vision and eye health:
Visual acuity test: This exam uses the Snellen eye chart to determine the smallest letters you can see on the standardized chart and measure how well you can see.
Visual refraction test: This test can determine whether you have a refractive error and the specific lens strength you need to correct it. It involves reading an eye chart while looking through a phoropter or refractor (an instrument with a group of lenses on each side).
Perimetry (visual field test): This test measures how wide of an area your eye can see, called your visual field, when you focus on a central point. It can help diagnose scotomas (blind spots) and loss of vision, which are indicators of glaucoma.
Slit lamp: This exam involves the use of a slit lamp (a microscope with a focused beam of bright light) that provides a magnified, three-dimensional view of your eye. It can help to diagnose a wide range of eye diseases and damage, including glaucoma.
Tonometry: This exam uses a device called a tonometer to inject puffs of air into your eyes to measure intraocular pressure. It can also test the effectiveness of glaucoma treatments.
Corneal topography: This exam takes thousands of pictures of your eye to examine the curve of your cornea. It can identify a curved cornea, which is called an astigmatism, and sources of swelling or scarring.
Ophthalmoscopy: Also called a fundoscopy, this exam involves shining a bright light into your eye to study your fundus (the back of your eye), which includes your retina, optic disc, and blood vessels.
Gonioscopy: This test uses a special lens and a mirror to measure your eye's drainage angle, where your iris meets your cornea, to identify if a blockage exists.
Learn More: Here’s What an Eye Exam Can Detect
Treatment for Pigment Dispersion Syndrome
If you have pigment dispersion syndrome with normal or only slightly elevated intraocular pressure, no treatment is typically prescribed because there is a low risk of optic nerve damage. You should maintain annual visits to your opthalmologist so they can monitor your condition and identify changes in your intraocular pressure or vision as early as possible.
When eye drainage canals are blocked and intraocular pressure increases, there is a higher risk of damage to your optic nerve. Treatment of pigment dispersion syndrome focuses on lowering your eye pressure because it is difficult to reduce or eliminate the release of iris pigment.
Factors such as the severity of your condition and your general health will determine which of the following types of treatment are appropriate:
Medications
The medications for treating pigment dispersion syndrome are the same prescription eye drops that can treat early glaucoma. These treatments are the most common early treatment for the condition. There are many options. You may be prescribed one or more of the following types of eye drops:
Alpha-adrenergic agonists: These drugs reduce the amount of fluid your eye produces and increase the amount of fluid that drains out of your eye. They include Iopidine (apraclonidine) and Alphagan P or Qoliana (brimonidine).
Beta-blockers: These drugs reduce the amount of fluid your eye produces. They include Betoptic (betaxolol) and Betimol, Istalol, or Timoptic (timolol).
Carbonic anhydrase inhibitors (CAIs): These drugs reduce the amount of fluid your eye produces. They include Trusopt (dorzolamide) and Azopt (brinzolamide).
Prostaglandin analogs: These drugs increase the drainage of fluid out of your eye. They include:
Xalatan (latanoprost)
Travatan Z (travoprost)
Zioptan (tafluprost)
Lumigan (bimatoprost)
In some cases, an older drug called Isopto Carpine (pilocarpine) is prescribed to treat the disease. This drug is in a class called miotics. It constricts (reduces the size) of your pupil (the black, round center of your iris) to increase the amount of fluid that drains out of your eye.
However, pilocarpine can also increase your risk of retinal detachment, a condition for which people with myopia (a common condition in pigment dispersion syndrome) are already at risk.
Surgery
Conventional surgery for pigment dispersion syndrome involves removing a small piece of tissue to make a new opening, or channel, for fluid to leave your eye. It is typically reserved for use after medications and laser surgery fail to improve your condition.
Laser Treatment
Laser treatment for pigment dispersion syndrome can involve one of the following procedures:
Laser trabeculoplasty: This treatment uses a laser to improve eye canal drainage and lower pressure. The procedure involves making several evenly spaced burns that stretch the drainage holes in the existing meshwork. The extra holes can improve fluid drainage from your eye.
Laser peripheral iridotomy: This treatment involves using a laser light beam to burn a microscopic hole in your iris to help widen the pathway to the drain of your eye. This allows for the free movement of fluid within the front section of your eye so the fluid can drain more easily.
Lifestyle Interventions
The following lifestyle interventions may reduce your risk of increased intraocular pressure:
Avoid certain yoga positions. Avoid yoga positions that require placing your head below or at a level with your heart, which can trigger higher intraocular pressure.
Limit the playing of certain wind instruments. Practice caution when playing certain wind instruments such as the bagpipes, the trombone, or the trumpet. Playing these types of instruments increases pressure around your face and upper airway, which can increase intraocular pressure.
Avoid small eye goggles. Avoid wearing swimming goggles that sink inside your eye socket, which can increase intraocular pressure during wear. Opt for larger snorkeling-type goggles that exert less eye pressure.
Don't wear tight neckwear. Avoid wearing shirts with tight collars or tight neckties. Tight neckwear can raise pressure in the veins of your head and neck, leading to an increase in intraocular pressure.
Learn More: How Glaucoma Is Treated
Can You Prevent Pigment Dispersion Syndrome?
Preventing pigment dispersion syndrome may not be possible because the condition is affected by unmodifiable factors such as genetics and eye structure. However, you may be able to manage the condition and reduce your risk of complications with the following strategies:
Get regular eye examinations. Regular eye examinations by an eye professional are essential for early detection and better outcomes. This is especially important if you have a family history of pigmentary dispersion syndrome or other types of glaucoma.
Maintain a healthy lifestyle. A healthy lifestyle includes following a balanced diet, participating in regular exercise, and establishing and maintaining a healthy weight. These factors can support overall eye health and help manage pigment dispersion syndrome.
Limit caffeine. There is evidence that intraocular pressure increases for about two hours after drinking coffee and other caffeinated beverages. Caffeine can also increase the production of aqueous fluid in your eye. Consider limiting your caffeine to a safe intake of 3 to 5 cups per day. Decaffeinated beverages may be safer options.
Avoid activities that are known to increase intraocular pressure. High-impact sports, strenuous exercise, and heavy weightlifting can cause rapid eye dilation. This can trigger the release of pigment granules, which can accumulate and increase intraocular pressure. Typically, low-impact exercises like walking or swimming can be done safely.
Wear proper eye protection. Reduce your risk of eye injuries that could worsen pigment dispersion syndrome. Wear eyewear that provides appropriate protection during sports or other activities that involve a high risk of eye injury. Look for protection that includes high-impact-resistant polycarbonate lenses and padded sports goggles.
What's the Outlook for Someone With Pigment Dispersion Syndrome?
Early diagnosis and appropriate treatment can support an excellent outlook for most people with pigment dispersion syndrome. Eye-pressure-lowering medications can successfully decrease fluid in your eye or increase fluid drainage out of your eye. Laser treatments or surgery are options for more severe cases. Vision loss is relatively rare.
Pigment dispersion syndrome may also regress over time and improve with age. This has been noted in mostly younger patients. In these cases, there are also reports of people experiencing a return to normal eye pressure.
Complications and Associated Conditions
Without proper treatment and relief of increased intraocular pressure, pigmentary dispersion syndrome can lead to the following complications.
Pigmentary Glaucoma
Glaucoma is a group of eye diseases that produce increased intraocular pressure as a result of backed-up fluid in your eye.
Pigmentary glaucoma occurs when pigmentary dispersion syndrome results in damage to your optic nerve. Your optic nerve contains the nerve fibers that carry visual messages from the back of your eye to your brain. Damage to your optic nerve can lead to permanent vision loss.
Up to 35% of people with pigmentary dispersion syndrome eventually develop high intraocular pressure or pigmentary glaucoma.
Cataracts
While cataracts (clouding of the eye lens from clear to yellow) are not a common complication of pigmentary dispersion syndrome, there is evidence of an association between the disease and cataracts that affect the nucleus, or center, of the eye's lens. These cataracts are categorized as nonsenile cataracts because they are not age-related.
Summary
Because it can occur without symptoms and affect young adults, pigment dispersion syndrome is an underdiagnosed disease. The precise cause of this disease is unknown. However, factors such as family history, age, and high myopia can increase your risk.
Treatment aims to reduce the increase in eye pressure caused by extra fluid. Based on your symptoms and disease state, therapies include prescribed eye drops, laser therapy, or surgery.
Having yearly eye exams can help you find pigment dispersion syndrome early. Contact an eye expert without delay if you notice any vision changes. Getting an early diagnosis and following prescribed treatments can help protect your eye health and prevent vision loss.
Read the original article on Verywell Health.

