Non-Blanching Rash: Causes and When to Call a Healthcare Provider
Non-blanching rashes can be a sign of serious illness, but not always
Medically reviewed by Brendan Camp, MD
A non-blanching rash is a type of rash that doesn’t disappear (or blanch) when pressure is applied. This is opposed to typical rashes, which return the skin to its natural color or a lighter shade when pressed.
Non-blanching rashes, also known as petechial rash, are caused by blood vessels bleeding under the skin. A rash that doesn’t itch or hurt in adults or children is often non-blanching. These rashes can indicate serious illness, including meningitis, sepsis, and leukemia. Anyone with a non-blanching rash should call their healthcare provider.
Continue reading to learn about non-blanching rashes, including the differences between petechiae and purpura, how to conduct the meningitis glass test, and when petechiae or a non-blanching rash are concerning.
When to Worry About a Non-Blanching Rash
Non-blanching rashes can be a sign of serious illness, including meningitis. All children with a non-blanching rash should see a healthcare provider the same day, even if they do not have a fever.
If you’re an adult with a non-blanching rash, call your healthcare provider. Remember, a non-blanching rash isn’t always a sign of serious illness, but it’s best to err on the side of caution.

Anastasiia Stiahailo / Getty Images
Defining Non-Blanching Rash
A non-blanching rash is one that stays even when pressure is applied to the skin. This is the opposite of a blanching rash, which temporarily disappears or turns the skin lighter than or to its original skin tone when pressure is applied.
The most common type of non-blanching rash is made up of petechiae, which are caused by blood vessels breaking under the skin. Petechiae are:
Flat
Small, like a pinprick
Red, purple, or brown in color
Not itchy
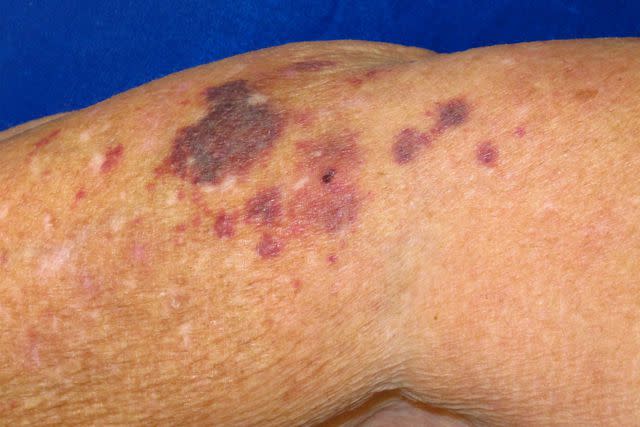
Another type of non-blanching rash is called a purpuric rash. This rash is made up of spots called purpura, which look like large bruises on the skin.
The difference between petechiae and purpura is minor compared to the fact that both can be a sign of meningitis, and require immediate medical attention.

Reproduced with permission from © DermNet dermnetnz.org 2023.
Reproduced with permission from © DermNet and © Te Whatu Ora dermnetnz.org 2023.
Compared to Blanching Rash
A blanching rash turns white or the color of your skin or lighter when pressure is applied. Blanching rashes are generally less serious than non-blanching rashes. However, some types of blanching rashes, like hives, can still be serious and require medical attention.
In addition, blanching of the skin can be a sign of circulation issues. This includes frostbite (injury to the skin and underlying tissue caused by from freezing temperatures).
Determining Whether a Rash Is Non-Blanching
To determine whether a rash on you or someone else is non-blanching, use this test, sometimes called the meningitis glass test:
Get a clear glass or container.
Gently push the side of the glass on the affected area of skin.
Look through the glass.
If you still see small marks while the glass is pushed against the skin, the rash is non-blanching. If the marks disappear temporarily and the area turns white, a lighter color, or skin toned, the rash is blanching.
Non-Blanching Rash in Meningitis
A non-blanching rash can be a sign of meningitis, an infection of the brain and spinal cord. Meningitis is most common in children and infants, so if your child has a non-blanching rash, call your healthcare provider immediately, even if they don’t have other symptoms.
Not all people with meningitis will develop the rash. The main three symptoms of meningitis are:
Mild fever
Stiff neck
Confusion
Emergency Symptoms
Meningitis is always a serious condition that requires immediate medical care. Call your healthcare provider if you or your child experiences these symptoms:
A non-blanching rash
Neck pain
Headache
Muscle aches and back pain
Nausea and vomiting
Fatigue and sleepiness
Non-Blanching Rash in Sepsis
A non-blanching rash can also be a sign of sepsis, a serious, body-wide reaction to an infection. Sepsis often occurs after another illness, including pneumonia and skin, gut, or urinary tract infections. It’s always a medical emergency that requires immediate care.
Emergency Symptoms
Sepsis is always an emergency, so contact your healthcare provider immediately if you experience these signs and symptoms of sepsis:
Fever and chills
Clamminess on the skin
Shortness of breath
Pain or discomfort
A non-blanching rash
Other Non-Blanching Rash Causes
There are many other causes of non-blanching rash, some of which are serious and some of which are less so. People with leukemia, a type of blood cancer, are more prone to broken blood vessels. They can develop a rash called leukemia petechiae.
Other causes of non-blanching rash can include:
Viral illnesses, including chickenpox
Henoch-Schönlein purpura (HSP), an autoimmune disorder
Immune thrombocytopenic purpura (ITP), a blood disease
Bumps, scrapes, and physical causes
Physical abuse
How Non-Blanching Rash Looks
A non-blanching rash often starts off looking like pinpricks on the skin that may appear red, brown, or purple. As the rash continues to spread, the spots may join together and look like bruising.
Location
Non-blanching rashes appear most often on the arms and legs, but can also develop on the torso and elsewhere on the body.
Onset of Symptoms
Non-blanching rashes often appear suddenly. If left untreated, they will progress, covering more of the skin until the skin appears to have large bruises.
Appearance and Shape
Petechiae appear like small pinpricks on the skin, which may look red, brown, or purple. Purpura appear like bruises, and can become quite dark.
Sensations
Non-blanching rashes typically don’t itch or hurt. However, many of the underlying conditions leading to non-blanching rashes can cause aches and pains, so you may experience discomfort.
Untreated Complications From Non-Blanching Rash
Some of the conditions that can cause a non-blanching rash, like meningitis and sepsis, can be fatal if left untreated. It’s important to reach out to your healthcare provider immediately if you’re experiencing a non-blanching rash so that they can provide treatment and avoid potentially deadly complications.
Non-Blanching Rash Treatment
The first step to treating a non-blanching rash is to determine the root cause. Once healthcare providers know what’s causing the rash, they can treat the underlying condition and the rash should revolve.
Understanding Non-Blanching vs. Blanching Rash Severity
In general, non-blanching rashes are considered more serious than blanching rashes. That’s because non-blanching rashes are associated with serious conditions including meningitis, sepsis, and leukemia. In general, blanching rashes have less serious causes, like skin irritations.
However, hives are a type of blanching rash that can still be quite serious if they appear as part of an allergic reaction. When in doubt, always call your healthcare provider whether your rash is blanching or non-blanching.
Summary
A non-blanching rash is one that does not go away when pressure is applied. Non-blanching rashes are caused by broken blood vessels beneath the surface of the skin. Often, the causes of a non-blanching rash aren’t serious.
However, these rashes can be caused by very serious, even deadly, infections, including meningitis and sepsis. In other cases, they can be a sign of leukemia. If you have a non-blanching rash, talk with your healthcare provider immediately, even if you don’t have other symptoms.
Read the original article on Verywell Health.

