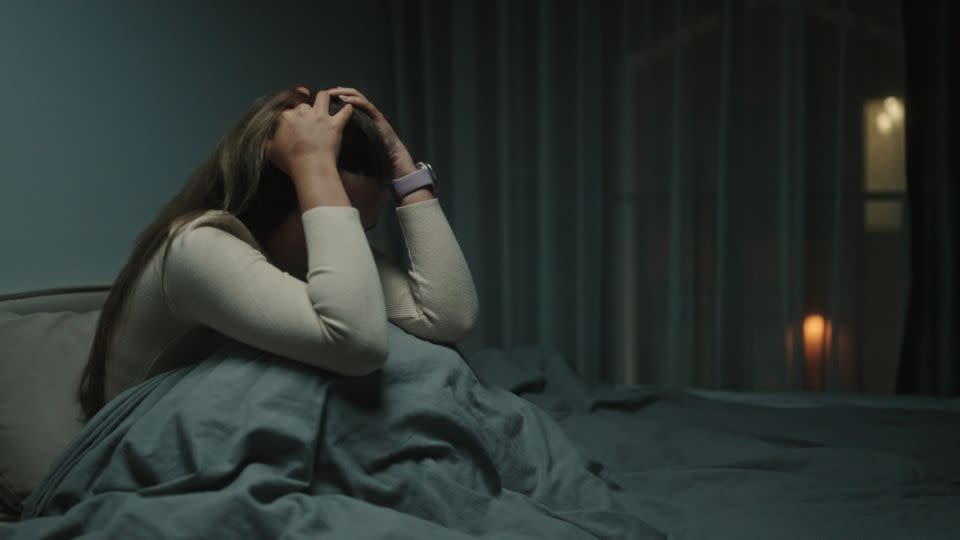
Horrific nightmares may signal initial onset of these chronic diseases, study says

Sign up for CNN’s Sleep, But Better newsletter series. Our seven-part guide has helpful hints to achieve better sleep.
The nightmares are intense and often horrifying, sometimes lasting well into the day.
“There’s a serial killer after me and the last few years I have the same one,” according to a Canadian patient. “He’s got my legs or something I can still feel something on my legs even when I’m then awake.”
Another English patient described nightmares “where I can’t breathe and where someone is sitting on my chest.” Yet another shared stories of “really nasty” violent visions in their sleep.
“Horrific, like murders, like skin coming off people,” said one Irish patient about his nightmares. “I think it’s like when I’m overwhelmed which could be the lupus being bad … so I think the more stress my body is under then the more vivid and bad the dreaming would be.”
Nightmares and “daymares,” dreamlike hallucinations that appear when awake, may be little-known signs of the onset of lupus and other systemic autoimmune diseases such as rheumatoid arthritis, according to a new study published Monday in the journal eClinicalMedicine.
Such unusual symptoms may also be a signal that an established disease may be about to intensely worsen or “flare” and require medical treatment, said lead study author Melanie Sloan, a researcher in the department of public health and primary care at the University of Cambridge in the United Kingdom.
“This is particularly the case in a disease like lupus, which is well known for affecting multiple organs including the brain, but we also found these patterns of symptoms in the other rheumatological diseases, like rheumatoid arthritis, Sjogren’s syndrome, and systemic sclerosis,” Sloan said in an email.
Lupus is a long-term disease in which the body’s immune system goes haywire, attacking healthy tissue and causing inflammation and pain in any part of the body, including blood cells, the brain, heart, joints and muscles, kidneys, liver, and lungs.
“Cognitive problems and many of these other neuropsychiatric symptoms we studied can have a huge influence on people’s lives, ability to work, to socialize, and just to have as much of a normal life as possible,” she said.
“These symptoms are often invisible and (currently) untestable but that shouldn’t make them any less important to be considered for treatment and support.”
Jennifer Mundt, an assistant professor of sleep medicine, psychiatry and behavioral sciences at Northwestern University’s Feinberg School of Medicine in Chicago who was not involved in the study, said in an email she was pleased the study focused on nightmares.
“Although nightmares are a very distressing problem in many medical and psychiatric conditions, they rarely get focused on except in the context of PTSD (post-traumatic stress syndrome),” Mundt said.
“A recent study showed that 18% of people with long-COVID have (frequent) nightmares, and this compares to a general population prevalence of about 5%,” she said. “Hearing the patient perspective is critical so that research and clinical care can be guided by what is most important to patients themselves.”
Doctors and patients need to know
While research in the field is rather new, a March 2019 study found patients with inflammatory arthritis and other autoimmune and inflammatory diseases also experienced nightmares and other REM sleep disorders such as sleep paralysis. REM is short for rapid eye movement, the stage of sleep in which people dream and information and information and experiences are consolidated and stored in memory.
In that study, one 57-year-old man recalled being “threatened by feral birds of prey” in his nightmares, while a 70-year-old woman dreamed her nephew was in grave danger but she could do nothing to help him.
The new study surveyed 400 doctors and 676 people living with lupus and also conducted detailed interviews with 50 clinicians and 69 people living with systemic autoimmune rheumatic diseases, including lupus.
Researchers found 3 in 5 lupus patients, and 1 in 3 patients with other rheumatology-related diseases, had increasingly vivid and distressing nightmares just before their hallucinations. These nightmares often involved falling or being attacked, trapped, or crushed or committing murder.
“I’d be riding a horse, going around cutting people out with my sword. One of them was somebody attacking me and I ended up slitting their throat,” the English patient said.
“I’m not a violent person at all. I don’t even kill an insect,” the patient continued. “And I came to the conclusion that’s probably me fighting my own (autoimmune) system. … I’m probably attacking myself, that’s the only thing I can logically make sense out of it.
Systemic autoimmune diseases often have a range of symptoms, called prodromes, that appear as signs of a sudden and possibly dangerous worsening of the condition. In lupus, for example, headaches, an increase in fatigue, painful, swollen joints, rashes, dizziness and a fever without an infection are well-known signs of an upcoming flare.
Recognizing these warning signs are important, Sloan said, because they allow “earlier detection and therefore treatment of flares, some of which can be organ damaging and even fatal in lupus patients.”
However, unique warning symptoms such as nightmares and daymares are not in the diagnostic criteria for lupus or other diseases, Sloan said. The study found doctors infrequently ask about such experiences, and patients often avoid talking about them to their physicians.
“We are strongly encouraging more doctors to ask about nightmares and other neuropsychiatric symptoms — thought to be unusual, but actually very common in systemic autoimmunity — to help us detect disease flares earlier,” said senior study author David D’Cruz, a consultant rheumatologist at Guy’s Hospital and Kings College London.
Connect the dots to autoimmune disease
On first glance, it would make sense that such neurological manifestations as nightmares would occur if the autoimmune disease impacts the brain, which lupus often does, Sloan said. But that’s not what the study uncovered.
“Interestingly, we found that lupus patients who were classified as having organ involvement other than the brain, such as kidneys or lungs, often also reported a variety of neuropsychiatric symptoms in the lead up to their kidney/lung flare,” Sloan said via email.
“This suggests that monitoring these symptoms — such as nightmares and changing mood — as well as the usual rashes and protein in the urine (due to inflammation in the kidneys), etc., may help with earlier flare detection in many patients, not just those who go on to develop major brain involvement,” she said.
However, there is no reason for people with occasional nightmares or daytime dreams to be worried they may have an inflammatory autoimmune disease, said sleep disorder specialist Dr. Carlos Schenck, a professor and senior staff psychiatrist at the Hennepin County Medical Center at the University of Minnesota in Minneapolis.
“This study could alarm the general public into believing or worrying about whether they have lupus or a related autoimmune disorder if they have nightmares or hallucinations, which are what doctors call ‘nonspecific symptoms,’ meaning that a variety of conditions (medical and psychiatric) can manifest with these symptoms,” Schenck said in an email.
It is indeed “perfectly normal” to have occasional nightmares and even daymares, or hallucinations, which “are also more common than we think,” Sloan said.
However, if those are intense, upsetting and occur around other symptoms such as extreme fatigue, headaches and other signs of autoimmune disorders, they “should be discussed with a doctor,” Sloan said.
“People shouldn’t be afraid or embarrassed to talk about these symptoms,” she said. “In some cases, reporting these symptoms earlier, even if they seem strange and unconnected, may lead to the doctor being able to ‘join the dot’s’ to diagnose an autoimmune disease.”
For more CNN news and newsletters create an account at CNN.com

