This bacteria is getting harder for kids to fight
When 6-year-old Logan Peon got an ear infection last year, his pediatrician in Chicago gave him antibiotics. That should've been the end to a typical childhood illness.
But Peon had acquired a drug-resistant bacteria called Pseudomonas aeruginosa. Round after round of antibiotics failed to clear up the boy's painful infection and left him sick from side effects.
"It didn't matter what we did, we couldn't get rid of it," his mother Katie Fearon recalled.
SEE ALSO: Bacteria in our mouths may hold clues about why people get migraines
Her son eventually went to the hospital this fall to receive antibiotics intravenously. Fearon said she hopes this will finally do the trick. "It's just relentless," she told Mashable.
Drug-resistant infections like Peon's are rising among U.S. children, according to a new study in the Journal of the Pediatric Infectious Diseases Society.

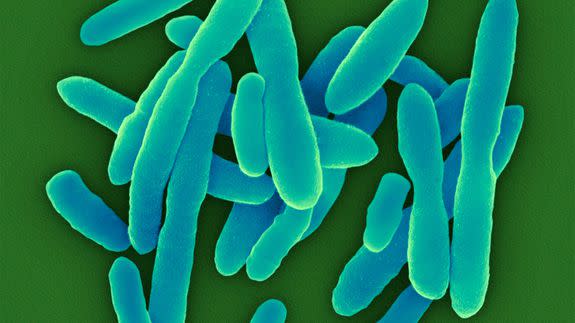
Image: tom boyle/Getty Images
Researchers found increasing rates of antibiotic resistance among samples of P. aeruginosa collected from pediatric patients nationwide. Left on their own, these infections can lead to severe illnesses, longer hospital stays and raise the risk of death.
"It's becoming more complex and difficult to treat," said Latania Logan, a co-author of the study and a pediatric infectious disease specialist at Rush University Medical Center in Chicago.
Globally, infections such as pneumonia and tuberculosis are becoming harder to treat across the board as antibiotics grow less effective. The World Health Organization now lists antibiotic resistance as one of the biggest threats to global health.
Too many prescriptions
The main reason for this scary trend is that we're taking too many antibiotics. Doctors might prescribe the pills as a catch-all cure when no treatment, or a different medication, is more appropriate. Patients similarly expect their doctors to prescribe antibiotics for whatever ails them. Or they might self-medicate or share leftover pills.
In addition, there has been a shift toward using large amounts of antibiotics in the livestock industry, which is also increasing the incidence of drug resistant bacteria.
By reducing the collective use of antibiotics, we could help reduce the spreading of highly resistant bacteria, doctors say. Until then, children like Peon may be increasingly at risk of hard-to-treat infections.

Image: Joe Raedle/Getty Images
For the study, Dr. Logan and her co-authors analyzed clinical data from about 300 hospitals nationwide for the years 1999 to 2012.
P. aeruginosa infections are fairly common among people with cystic fibrosis, a life-threatening disorder, so the researchers did not include those patients. The team studied samples from patients ages 1 to 17 who were in various health care settings at the time, such as an intensive care unit or in outpatient treatment.
While healthy people can acquire the bacteria, P. aeruginosa is more prone to attack patients who already have a compromised immune system. Six-year-old Peon, for instance, has always been prone to infections and is often at the hospital, where he may have picked up the ear infection, his mother said.
The researchers found the proportion of bacterial stains that are resistant to at least three classes of antibiotics rose from 15.4 percent in 1999 to 26 percent in 2012. The proportion of strains resistant to carbapenems — a class of antibiotics considered a treatment of last resort for highly resistant infections — rose from 9.4 percent to 20 percent.
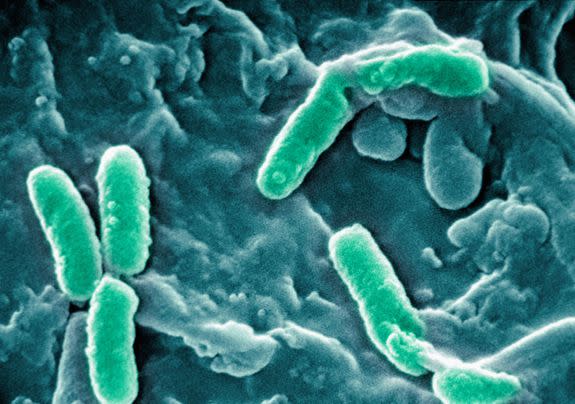
Image: Cultura/ap images
Drug resistance was most common in teenage patients, ages 13 to 17, and more prevalent in the Midwest, according to the Nov. 17 study.
The research is the first to examine national trends in P. aeruginosa infections.
Roberto Posada, a pediatrics specialist who was not involved in the research, said the findings provide important insight for medical professionals and families trying to understand the rising threat of drug-resistant infections.
Growing resistance to carbapenems in particular "has serious consequences" for infections in children, said Posada, who is a professor at the Icahn School of Medicine at Mount Sinai in New York City.
Logan said she hoped the findings would help get the word out to not only researchers but also nurses, home health care providers and other caregivers of sick children who may be at a higher risk of acquiring these serious infections.
"I don't know that people are as aware of how threatening this problem really is," she told Mashable.
BONUS: Smartphone cameras now have the power to detect anemia with this brilliant app
