What Is Ankylosing Spondylitis (AS)?
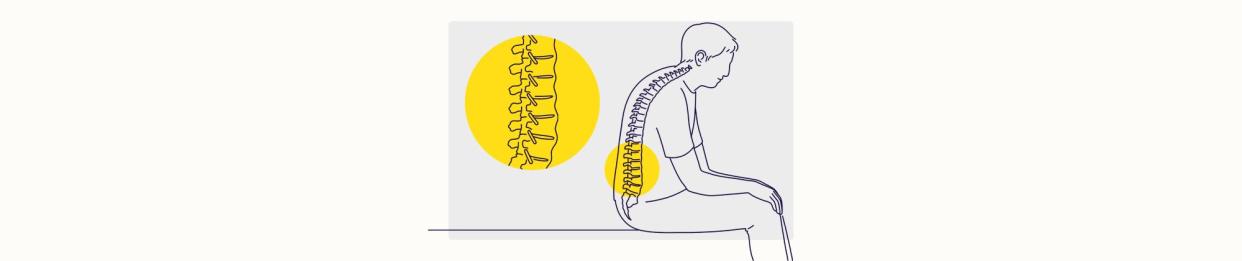
Illustration by Mira Norian for Health
Medically reviewed by Stella Bard, MD
An ankylosing spondylitis (AS) diagnosis means you have an autoimmune disorder and type of inflammatory arthritis. AS primarily affects the spine, causing symptoms like back pain and stiffness. Inflammation can change the structure of your joints, affect your posture, limit your range of motion, and reduce your quality of life.
The exact cause of AS is not fully understood. Some evidence suggests that a combination of genetic and environmental risk factors plays a role. If you think you may have AS symptoms, it's a good idea to get tested. A healthcare provider will learn about your medical history, perform a physical exam, and order additional tests (e.g., blood, imaging, or lab) to confirm AS.
There's no cure for AS, but treatment can help you manage your symptoms and improve your daily life. Read on to learn about AS symptoms, causes, treatments, and more.
Related: What Is Psoriatic Arthritis?
Ankylosing Spondylitis Symptoms
AS symptoms vary from person to person and can range from mild to severe. Symptoms usually appear before age 45 and develop gradually over time. Many people with AS have flares, or periods when symptoms worsen.
Common AS symptoms include:
Back pain and stiffness: These are the hallmark symptoms of AS. Spinal or back pain and stiffness are usually worse in the morning or after long periods of inactivity.
Enthesitis: Swelling and tenderness in the entheses mostly affect the heels, soles of the feet, and hips. The entheses are where your tendons and ligaments attach to your bone.
Fatigue: Inflammation and the side effects of medications can lead to chronic fatigue, or severe tiredness.
Joint pain: Inflammation can cause pain and stiffness in other joints, including the hips, shoulders, neck, ribs, knees, and feet.
Limited mobility: The spinal vertebrae (a series of small bones) can become stiff as the spine and other joints become more inflamed. This can reduce your range of motion and limit your ability to perform daily tasks.
Uveitis: This is inflammation of the eyes. Uveitis can cause redness, pain, light sensitivity, and vision changes.
You may also experience more severe symptoms as AS develops. These symptoms can include chest pain, difficulty breathing, digestive problems, and skin rash. Some people have anemia (a lack of oxygen-rich red blood cells), depression, or kyphosis (hunchback posture).
What Causes Ankylosing Spondylitis?
AS is an autoimmune disorder, meaning the immune system mistakenly attacks healthy cells in the spine. As a result, the immune system produces inflammation, which causes physical symptoms.
Researchers do not know the exact cause of AS. Some evidence suggests that a combination of genetic and environmental factors may be the culprit. People who have a family history of AS are more likely to develop it than others. Inheriting certain genes can contribute to your risk of AS and severity of symptoms.
Researchers have identified over 60 genes linked to AS. The most common gene in people with AS is the HLA-B27. Not everyone who has the HLA-B27 gene will develop AS. Genes alone do not cause AS. The interaction between your genetic makeup and environmental factors can trigger symptoms.
Risk Factors
Several risk factors can increase your risk of AS. These risk factors include:
Age: Most people with AS receive their diagnosis before age 40.
Inflammatory bowel disease (IBD): Crohn's disease, ulcerative colitis, or another disease that causes inflammation of the digestive system increases the risk of AS.
Mechanical stress: Wear and tear on the joints can trigger your genes to produce inflammation.
Previous infection: A history of certain bacterial or fungal infections may trigger immune system dysfunction and lead to the onset of AS symptoms.
Smoking: Research has shown that smoking can lead to a more rapid onset of AS symptoms.
It's important to note that having one or more risk factors does not guarantee you'll get AS. It just means that your risk is higher.
How Is Ankylosing Spondylitis Diagnosed?
An AS diagnosis requires a medical history and physical exam. A healthcare provider will measure your vitals, check your spine for pain and tenderness, assess the range of motion in your joints, and examine your posture. AS can mimic symptoms of other arthritis-related conditions. A healthcare provider will administer diagnostic tests to confirm AS and rule out other diseases.
These tests may include:
HLA-B27 genetic test: Checks for the HLA-B27 gene, which is common in people with AS, using a blood sample
Magnetic resonance imaging (MRI): Takes detailed images of soft tissues in the body and looks for signs of inflammation in the joints
X-rays: Checks for bone loss or damage, osteophytes (bony growths), and fusion (joining) of the spinal bones
Treatments for Ankylosing Spondylitis
There is no cure for AS, so the goals for treatment are to reduce pain and inflammation, slow disease progression, and prevent complications. Your treatment plan will depend on your symptoms, severity of the disease, age, and lifestyle.
A healthcare provider will likely advise a combination of medications and therapies to help manage symptoms. They can work with a surgeon to identify if surgery can improve severe or advanced symptoms and quality of life.
Medications
Several types of medications treat AS. Everyone responds to treatment differently. It may take trial and error until you find the right combination to control symptoms.
Medications that treat AS include:
Corticosteroids: A healthcare provider can prescribe steroid medications on a short-term basis to relieve joint pain.
Disease-modifying antirheumatic drugs (DMARDs): These drugs suppress the immune system to reduce inflammation and pain. DMARDs are typically ineffective for back pain but can relieve pressure in the peripheral joints (e.g., the hips, knees, and ankles).
Interleukin-17 (IL-17) inhibitors: IL-17 inhibitors block the immune system from producing inflammation to reduce pain and swelling in the joints.
Non-steroidal anti-inflammatory drugs (NSAIDs): These drugs control inflammation to reduce pain and stiffness. Some NSAIDs are available over-the-counter (OTC), such as Advil (ibuprofen). A healthcare provider can prescribe a stronger NSAID if your body does not respond to OTC options.
TNF inhibitors (TNFi): TNF inhibitors block tumor necrosis factor-alpha (TNF-a). The immune system makes this protein, which causes inflammation.
Physical Therapy
Physical therapy is an essential part of treating AS. A healthcare provider will likely refer you to a physical therapist to help you learn ways to reduce symptoms. The physical therapist will work with you to develop a treatment plan based on your needs and goals.
Physical therapy aims to increase muscle strength and endurance, enhance your breathing, and help you maintain a healthy weight. Exercises that help achieve these goals include:
Balance exercises
Cardio workouts (e.g., walking or biking)
Stretching
Weightlifting
Surgery
Some people with advanced AS may need surgery if they have severe pain, joint deformities, spinal fractures, or infections. A healthcare provider will usually only advise surgery if your symptoms are severe and other treatments have failed.
The healthcare provider will likely consult a surgeon or rheumatologist before telling you about your surgical options. A rheumatologist specializes in the joints, muscles, and bones.
The most common surgical procedures for AS include:
Hip replacement: Removing part of the hip joint and replacing it with a prosthetic joint
Laminectomy: Taking pressure off the spinal cord and nerves to relieve weakness, tingling, and pain
Osteotomy: Cutting and reshaping the spinal bone to correct deformities, improve posture, and help restore flexibility
Spinal fusion: Joining two or more spinal vertebrae (a series of small bones) to stabilize your spine and relieve severe back pain
How To Prevent Ankylosing Spondylitis Flares
Living with AS means you may have flares, or periods when your symptoms become more severe. Flares may cause severe back pain, fatigue, mild fever, depression, and pain in other joints.
You can prevent the frequency of AS flares by:
Following your treatment plan as prescribed
Getting uninterrupted sleep at night
Managing stress with relaxation or breathing techniques
Quitting smoking
Get in touch with a healthcare provider if you notice your flares are getting worse. They can help you learn other prevention techniques or adjust your treatment plan to help you better manage symptoms.
Related Conditions
Approximately 80% of people with AS have one or more co-occurring health conditions. Related conditions include:
Depression: Living with AS can be difficult. Dealing with painful symptoms that hinder your daily activities can lead to depressive thoughts and moods. Some evidence suggests that inflammation and pain caused by AS can lead to depression.
Heart disease: Chronic inflammation can affect the heart. AS can increase the risk of heart attack, stroke, irregular heartbeat, high cholesterol, high blood pressure, and heart failure.
IBD: Research has found a strong link between gut inflammation and AS. About 10% of people with AS develop an IBD within 20 years after diagnosis.
Osteoporosis: You might experience bone loss or damage, which can increase your risk of developing weak bones and fractures.
Related: What Is Rheumatoid Arthritis?
Living With Ankylosing Spondylitis
Living with AS and painful symptoms can be as difficult. It's a good idea to be proactive about your health and see a healthcare provider if you notice symptoms or have a family history of AS. Follow your treatment plan if you receive an AS diagnosis. AS can affect each person differently. It's OK if it takes some time to find a treatment regimen that's right for you.
Stay in touch with a healthcare provider and update them about your symptoms. Let them know if you think your medications or therapies are not working. Research for AS is ongoing, so experts are learning about new, effective treatments.
Taking your medications as prescribed, getting regular exercise, and managing stress levels can help control symptoms. You can also find emotional support through support groups, spending time with loved ones, and doing hobbies you enjoy. With the right treatments, people with AS can expect to live full, happy lives.
For more Health.com news, make sure to sign up for our newsletter!
Read the original article on Health.com.

