After 3 years, an Anderson Township woman is still trying to fix her Mercy Health bill
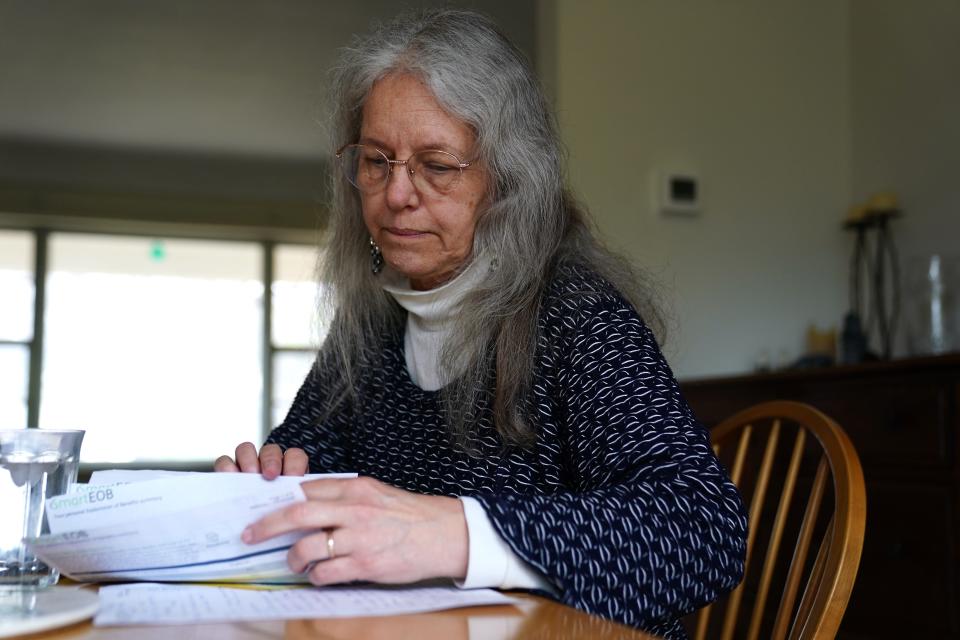
The Enquirer is investigating our readers’ medical bills. For this story, we talked to Martha Viehmann, 64, a woman from Anderson Township who received an unexpected bill in 2021 – and has been disputing it ever since.
If you have a medical bill you want us to check out, email it to ekim@enquirer.com.

The situation, in a snapshot
The patient: Martha Viehmann, 64, covered by her husband’s insurance through Humana at the time of the bill.
The medical service/device: A DEXA scan, a type of bone density test, in January 2021.
The service provider: Mercy Hospital Anderson.
The bill: Mercy Health charged Viehmann $1,045, which she now owes to the collection agency.
What happened? Viehmann’s doctor marked the bone scan as diagnostic instead of as a preventive service covered under the Affordable Care Act. Despite years of making calls, Viehmann couldn’t get Mercy Health to correct the claim, which the hospital sold to collections in 2022.
The outcome: The bill remains unpaid.
The lesson: Even with services defined as preventive under the Affordable Care Act, insurers still have significant power to determine what costs they’ll cover. And it is legal for a health care provider to sell a bill to collections, even if the patient is in the middle of disputing it. If you believe you’ve been billed unjustly, try enlisting the federal government’s help.
Martha Viehmann received the first call from the collection agency about her medical bill in November 2022. It was Thanksgiving week, and she was sick with COVID.
She remembers how much worse the call made her feel.
“I’m a good person. I don’t go into debt,” she remembers insisting to herself while fending off a sense of shame. She now owes collections $1,045, making her one of over 800,000 people in Ohio with medical debt, according to the Peterson-KFF Health System Tracker.
The service Viehmann was billed for was a DEXA bone scan she received in January 2021.
A DEXA bone scan is an X-ray that detects brittle bones and measures bone loss. It is recommended for postmenopausal women or women over the age of 65 to predict the odds of fracture.
This was Viehmann’s second scan. Her gynecologist ordered it to follow up on a previous scan from several years prior, which revealed that Viehmann had osteopenia, a condition preceding osteoporosis.

“They recommend that you take calcium supplements and increase your exercise,” said Viehmann, a part-time administrator from Anderson Township. “So the idea of the second bone scan was, well, how are you doing, Martha?”
HealthCare.gov lists a DEXA bone scan as a covered preventive service for postmenopausal women or women over the age of 65. But while Viehmann’s first DEXA scan was covered, she’s been disputing the bill for the second for over three years.
“For the first 18 months that I was trying to get this resolved, I was largely unemployed,” Viehmann explained when asked why she hasn’t given up after all this time. “Money was tight.”
Plus, her first scan had been covered. “I was convinced that I did not owe this.”

Provider, insurer disagree on preventive services
Dr. Sofia McCotter, Viehmann’s gynecologist at the Seven Hills Women’s Health Center in Anderson Township, ordered the bone scan. She labeled it as a diagnostic service instead of a preventive one.
The bone scan itself was performed at Mercy Health Anderson, a separate health care provider responsible for billing Viehmann for the service.
According to Viehmann, Humana representatives told her that Humana would cover the bill if Mercy Health submitted an updated claim with a preventive code. The Enquirer attempted to verify this account with Humana, but the insurance company did not respond to multiple requests for comment.
Ultimately, however, neither Seven Hills Women’s Health nor Mercy Health helped Viehmann update her claim.
Since Viehmann’s second screening followed her osteopenia diagnosis, McCotter was correct to categorize it as diagnostic, a representative from Seven Hills Women’s Health Centers told The Enquirer.
Viehmann heard something different when she called McCotter’s office and spoke to the person in charge of handling billing. “I remember this,” Viehmann said. “I almost sent it back to Dr. McCotter to have her change the code.”
Still, McCotter’s office directed Viehmann to Mercy Health’s billing department to resolve the issue. Viehmann said she waited for more than an hour on hold during her calls to Mercy Health in 2021.
Her objective remained the same: to get Mercy Health to submit a claim with a preventive code.
Finally, in August 2022, Mercy Health billing informed Viehmann that everything was resolved – then sold her bill to collections three months later.
Since then, Viehmann has continued to dispute her bill with Mercy Health, Humana and Capio Partners, the debt collection agency. “I kept calling to ask for a corrected claim,” said Viehmann, who estimated she’s made nearly 30 calls since 2021.
In February of this year, Humana told her that the deadline for processing her claim had passed.
Viehmann knows that the billing system that doctors navigate is complex, so she doesn’t blame McCotter for her situation. Yet she’s deeply frustrated by how challenging it has been to amend her claim, with little transparency from the companies she's contacted about the situation.
“I’m not in control. I know nothing about what’s going on,” Viehmann said. “It’s because of the clerical error that I’ve been told that I owe $1,000 to a collection agency.”
Mercy Health submits duplicate claims to Humana, doesn't explain why
Viehmann’s insurance documents, including explanations of benefits and a claim receipt, show that Bon Secours Mercy Health submitted three claims to Humana with the same diagnostic code. Humana rejected the latter two as duplicates.
The Enquirer reached out to Mercy Health and Humana to figure out why. While Humana did not respond to multiple requests for comment, Lisa Dyson, spokesperson for Bon Secours Mercy Health, responded, “We have collaborated with the patient’s physician to code the service accurately.”
Dyson didn’t explain when that happened or clarify why Mercy Health submitted three identical claims to Humana.
“The challenges this patient has experienced are an example of how insurance companies have added to the administrative burden placed on providers and hospitals in an effort to deny payment,” Dyson said.
It’s true that even for services clinically considered to be preventive, insurers can decide how much to cover, according to Krutika Amin, associate director of KFF’s program on the Affordable Care Act. KFF, formerly known as the Kaiser Family Foundation, is a nonprofit health policy research organization.
“Each insurance has their own rules,” Amin said. “There’s still a lot of leeway there as to how plans interpret that.”
It's also not uncommon for billing errors to get sold to collections. It’s legal for hospitals do so because there is no federal law that prevents providers from collecting an outstanding balance, even if patients like Viehmann are actively trying to dispute their bill.
Got a surprise charge? The federal government might investigate
For patients surprised by out-of-network charges on their medical bills, Amin recommends filing a complaint with the No Surprises Help Desk. It's part of the Centers for Medicare and Medicaid Services, a federal agency that investigates medical bills violating federal law.
You can submit your bill online, or call 1-800-985-3059 to reach the Help Desk, which also offers services in Spanish and over 350 other languages.
The federal government can investigate and fine insurers and health care providers for incorrectly billing patients. As of October 2023, they have paid out $3 million in monetary relief as a result of their investigations.
If Viehmann has taken anything away from this experience, it’s empathy for others in her situation.
“I absolutely understand why people drag their feet,” Viehmann said. “They don't want the bad news. They’re afraid of the bills.”
Have a medical bill you want The Enquirer to investigate? Fill out this form to let us know. This was inspired by the Bill of the Month series, a joint investigation from KFF Health News and NPR.
This article originally appeared on Cincinnati Enquirer: Mercy Health said her bill was resolved. Then collections called

