Here’s Why Your Teeth Really Hurt and How to Stop the Ache, According to Dentists
Whether you’ve got a sudden, sharp pain in one tooth that makes chewing all but impossible or a dull, throbbing ache you can’t quite ignore, a toothache can be seriously distracting and painful—and getting rid of yours is probably top of mind.
So why do your teeth hurt, exactly? “Tooth pain can be caused by a whole host of factors beyond just conventional cavities and the insatiable sweet tooth,” says David Frank, D.M.D., a cosmetic dentist and owner of Walden Dental in Austin and Cedar Park, Texas. “Dental trauma, tooth fractures, gum and bone disease, TMJ disorders, and impacted wisdom teeth can all contribute to a toothache.”
In an ideal world, you’d see your dentist for a check-up, cleaning, and preventative dental care every six months to help avoid major toothaches. However, if that hasn’t been a possibility lately, you’re far from alone. About 48% of adults don’t make it in to see the dentist that often due to barriers like cost, fear of the dentist, and the inability to find a convenient location of appointment time, per the American Dental Association (ADA).
Unfortunately, the longer you wait to treat tooth pain, the more invasive, costly, and painful treatments tend to be, says Vanessa Creaven, M.F.D.S, CEO and co-founder of Spotlight Oral Care, an oral health products company. For this reason, it’s key to get in to see your dentist as soon as you can if you’ve got a nagging toothache and want to avoid a dreaded root canal or extraction, she says.
For a mild toothache, sometimes rinsing your mouth out with warm water and gently brushing and flossing your teeth can help ease your pain. That said, if you still have tooth pain a day or two later or you have other concerning symptoms like an unpleasant taste in your mouth, swollen gums, or a fever, that’s your cue to call your dentist and schedule an appointment ASAP.
In the meantime, reading up on the topic can help ease your worries and prepare you for what to expect if and when you head into the dentist’s office. Here, nine possible reasons you teeth hurt and how to treat them, according to doctors.
1. You guessed it: You’ve got a cavity.
A random toothache, increased sensitivity, or sharp pain when you’re eating something sweet, hot, or cold could indicate that you have a cavity. Day-to-day dental care is arguably even more important as you get older, since as your gums recede, even larger spaces are left in between your teeth. There, bacteria, acid, food, and saliva can form plaque which in turn dissolves the enamel that protects your teeth and attacks your tooth structure, creating holes (a.k.a. cavities) in your teeth, explains Pia Lieb, D.D.S., founder of the Cosmetic Dentistry Center in New York City.
If you suspect you might have a cavity, a filling—a process which typically takes less than an hour—should do the trick. However, you may need a crown (which covers your entire tooth) or root canal (to remove and fill in the damaged part of your tooth) if your tooth decay is more extensive. After that, the best prevention is to brush and floss and keep up with regular dental appointments, as routine X-rays can reveal cavities in earlier stage before a toothache even strikes, says Dr. Lieb.
2. That filling you got is failing you.
If you’ve got short, sharp, or dull tooth pain in an area where you’ve already had a cavity treated, a damaged filling may be to blame. Made out of resin, porcelain, or other tooth-like materials, fillings can be disrupted by trauma to your tooth (like a hard hit to your face or biting down too hard on food) or decay in the surrounding area, says Dr. Creaven. Call up your dentist to let them know what’s going on, as you may need to have your filling adjusted or replaced entirely.
3. Your teeth have become more sensitive.
Sudden yet temporary tooth pain that pops up when you drink or eat certain things—like hot coffee or ice cream—often means that you’ve developed a hypersensitivity. Usually, this is a result of receding gums or brushing your teeth too hard, which could expose the root and nerve of your tooth or remove protective enamel from the outer layer of your tooth, says Dr. Lieb. Depending on your specific needs, your dentist will come up with a treatment plan that may include using a softer toothbrush and a desensitizing toothpaste, notes Dr. Creaven.
4. A cracked tooth could be the culprit.
A cracked tooth, which you may not be able to see with your naked eye, can trigger a sharp, shooting pain when you bite down or release a bite while chewing, says Dr. Frank. Often, this occurs due to trauma (like biting down too hard or grinding your teeth at night) or when large fillings put too much pressure on your tooth.
Treatment will depend on just how deep the crack in your tooth has gotten. In most cases, a new filling or crown should suffice to reinforce and protect your weakened tooth. But if the crack has extended to the nerve of your tooth—which can cause seriously severe pain—you may need a root canal or extraction, so call your dentist STAT, says Dr. Frank.
5. You’re taking your stress out on your teeth.
If you wake up with a sore jaw and aching facial muscles or find yourself clenching your teeth in the middle of a demanding workday, stress could be at the root of your toothache.
Sound familiar? Talk to your doctor about your symptoms and the type of pain you’re having, as grinding your teeth can sometimes cause significant damage like chipped or cracked teeth. Wearing a mouth guard could help ease your pain (and many are available over-the-counter), but you might also want to look into stress-reduction techniques like meditation or getting a sleep health check-up. As it turns out, teeth grinding can be associated with other sleep disorders such as sleep apnea, notes Umang Patel, D.D.S., a dentist at Romeoville Dental Center in Romeoville, Illinois.
6. It may be a sign of TMJ.
Sometimes, what seems like “tooth pain” is actually generalized jaw pain. If you have an imbalance in your temporomandibular joints (a.k.a. TMJ), you might experience mild discomfort while chewing or even total lockjaw with an inability to open or close your jaw, says Dr. Frank. It’s rare, however, that TMJ disorders will only feel like an individual toothache.
Treatment ranges from mouth guards and medication like pain relievers and muscle relaxants to full joint replacement. Early treatment is key, so make sure to contact your dentist to figure out what’s going on with your jaw, says Dr. Frank.
7. Your sinuses could be to blame.
While it might not be the first thing you think of when you have a toothache, pressure from inflamed sinuses or a sinus infection could cause dull tooth and facial pain (especially in your upper set of chompers, which are closest to your sinuses), says Dr. Patel.
Many self-care methods can help get your sinuses draining, so drink up, steam your face with a hot mug or water to thin out mucus, and consider taking an over-the-counter decongestant according to the label instructions. If you spike a fever, your pain shifts into severe territory, or your symptoms don’t go away after two weeks, contact a doctor for professional help, per the American Academy of Family Physicians (AAFP).
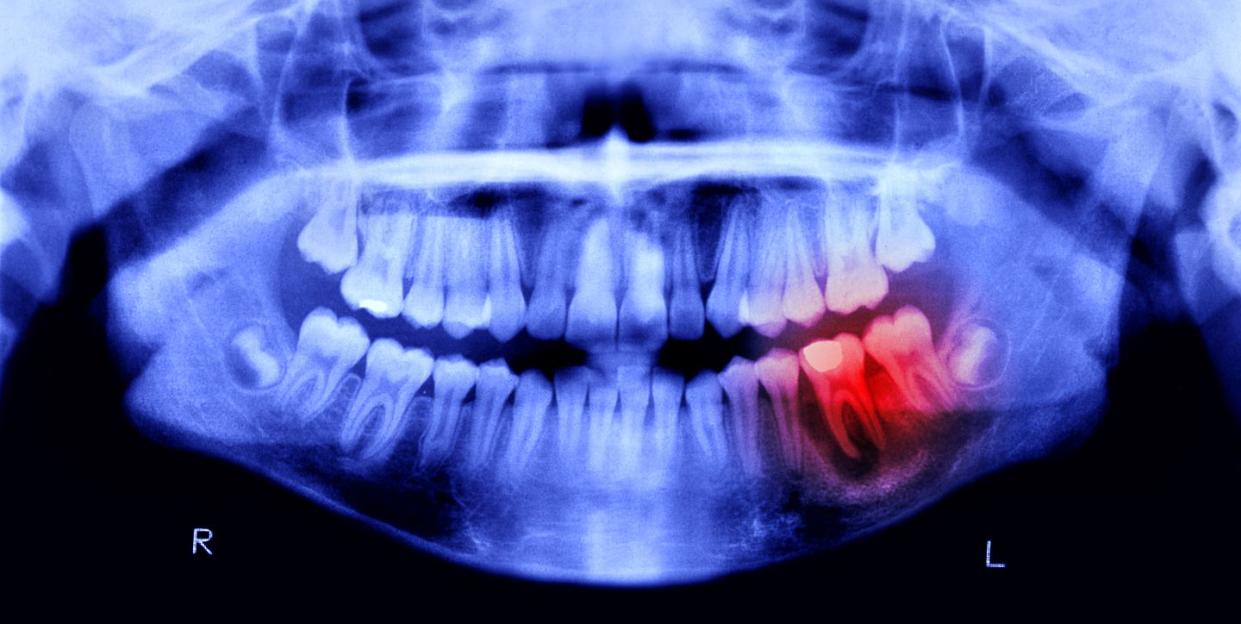
8. Your wisdom teeth are acting up.
Still got your wisdom teeth? Tooth pain in the back of your mouth that waxes and wanes could indicate a problem with them, says Dr. Frank. Impacted wisdom teeth that don’t have enough room to emerge can develop cavities, become infected, or damage nearby teeth, which, in turn, also increases the risk of infection, per the Mayo Clinic.
While there’s no way to change where your wisdom teeth choose to come up, a dental exam can help your dentist ID the problem and an oral surgeon can help you decide whether or not to remove them.
9. A tooth infection could be lurking.
A tooth infection can arise for a number of reasons, from recent dental work to an injury or untreated cavity, says Dr. Lieb. As a result, you may experience severe tooth pain along with gum swelling and irritation, bad breath, a bitter, salty taste in your mouth, and in some cases, a fever. If you have a bacterial infection, you may see a pus-filled “pimple” on your gum known as an abscess.
The only way to deal with a tooth infection is to remove the source, by extracting your tooth or performing a root canal, says Dr. Patel. As for medication, usually a combination of Advil (ibuprofen) and Tylenol (acetaminophen) can control the pain, though sometimes prescription pain medication and antibiotics are needed depending on how far your infection has progressed.
Support from readers like you helps us do our best work. Go here to subscribe to Prevention and get 12 FREE gifts. And sign up for our FREE newsletter here for daily health, nutrition, and fitness advice.
You Might Also Like

