Postpartum Depression 101: Everything You Need to Know About the Crazy Common Affliction
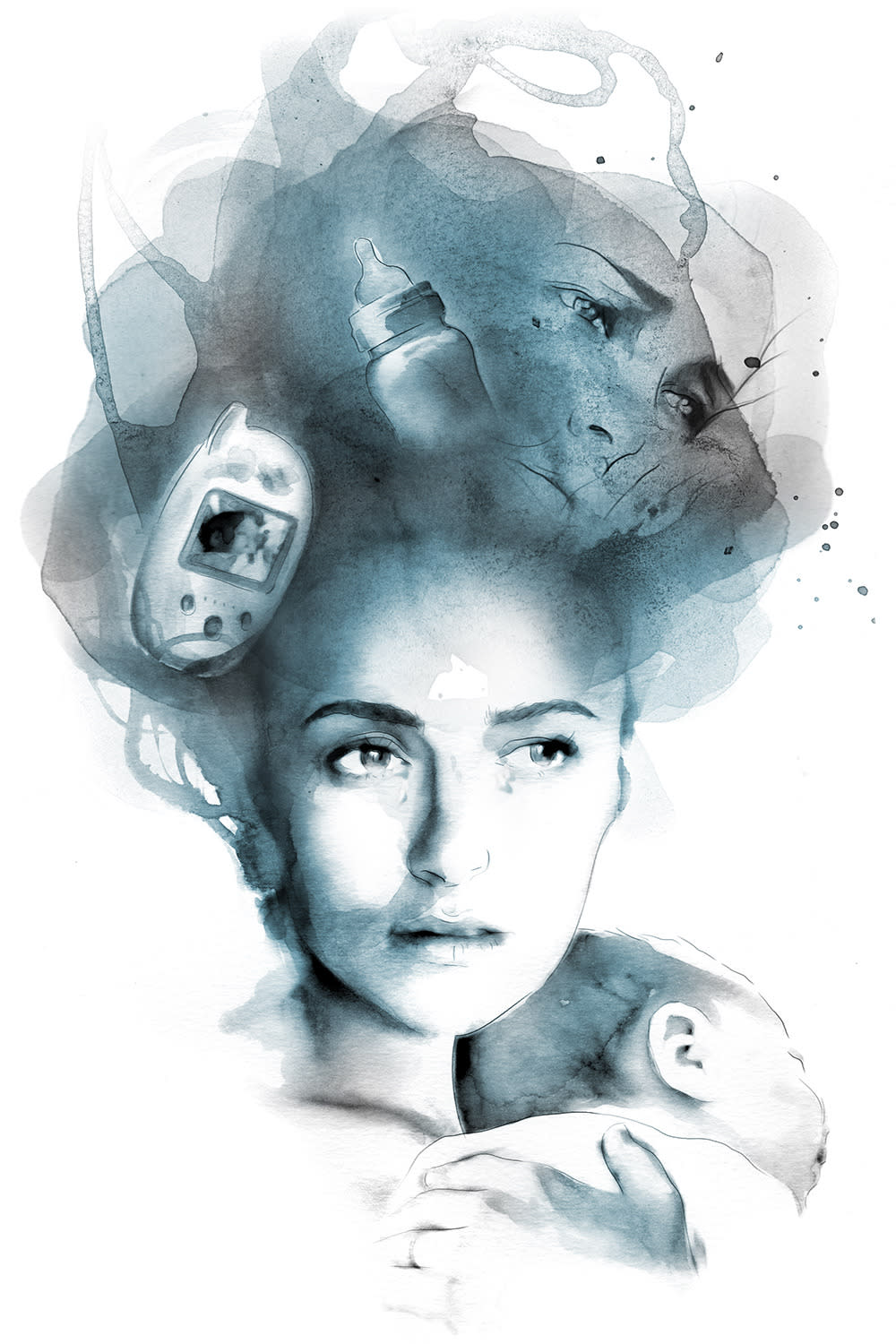
Illustration by Jaume Vilardell for Yahoo Style
Jen, now 41, was taking a quick, much-needed manicure break from new motherhood when she had her first postpartum anxiety attack. She’d given birth to her son less than two months before, and though she’d since noticed some unsavory changes—“not sleeping, crying a lot”—she initially wrote them off as little more than the baby blues.
It wasn’t until she was settled into the manicurist’s chair that the magnitude of her new responsibilities—her new life—truly hit her. “I had a panic attack,” Jen, an advertising director in L.A., recalls. “I was sweating, [and my] heart was beating fast. I did not want to go home; I physically could not go home.”
Postpartum symptoms like Jen’s are quite common, more so than the pervasive silence around them might have you believe. According to the American Psychological Association, PPD affects between 9-16 percent of new mothers, generally within the first year of giving birth. There’s no conclusive test to diagnose it, but some common symptoms are sadness, sleep disturbance, appetite changes, social withdrawal, and, per Dr. Juli Fraga, a San Francisco psychologist, “intrusive thoughts” about the baby’s safety. Like regular depression, PPD is treatable with talk therapy and medication, though the type of meds depend on whether the woman is breastfeeding. Left untreated, it can last for months or even years.
So recently when the actress Hayden Panettiere announced she would be seeking treatment and going on indefinite leave from her hit show Nashville, she helped drive this important but underreported issue of postpartum depression into the spotlight. Yes, even celebrities aren’t immune. Brooke Shields recalled considering suicide in her book, Down Came the Rain: My Journey Through Postpartum Depression; Amanda Peet admitted she dealt with a “fairly serious” bout of PPD after giving birth to daughter Frankie; and Gwyneth Paltrow once said she “didn’t feel anything” after giving birth to her son Moses in 2006. As Panettiere explained on Live! With Kelly and Michael, “[PPD is] something that needs to be talked about. Women need to know that they’re not alone.“
Indeed, sufferers of PPD are anything but alone, though one of the symptoms can be, well, feeling that way. Wendy, now 43, of Virginia, suffered from postpartum depression when she gave birth to both of her kids, and recalls, “When I had my daughter, I was fairly isolated with no immediate family [nearby]. All of my female friends still worked full time, so I didn’t have anyone [to talk to] during the day.” Though Wendy, a writer, had struggled with depression since childhood, after the birth of her kids she had a hard time reaching out for help because she “didn’t want to be judged.”
Wendy’s reluctance to open up about it isn’t unusual: our culture doesn’t exactly encourage transparency when it comes to women’s mental-health experiences. Especially ones that contradict the narrative that motherhood should unquestionably foster uncomplicated insta-happiness. In fact, many women feel such pressure to look and feel like “normal,” all-thrilled, all-the-time new moms that they don’t talk about their struggles at all.
Dr. Fraga says that some women’s reluctance to disclose these feelings is due to a sense of “shame that motherhood isn’t a more joyful time for them.” Instagram, Facebook, and a proliferation of gushy parenting blogs can make it all too easy to compare yourself and feel like you’re coming up short – especially when so many feeds are brimming with new moms swaddling their tots in designer duds or discussing the seemingly uncomplicated joy of breastfeeding. The reality for many new moms is less than pretty; they’re juggling confounding new responsibilities with little sleep, tight budgets, and bodies that have been through hell and back.
Given the massive hormonal shifts and sleep deprivation generally involved in new mamahood, it’s not always easy for women to differentiate between run-of-the-mill “baby blues” and something more serious. As Dr. Fraga says, “It’s a time of so much change, who wouldn’t be crying and snapping at their partners?”
Jen seconds that. She remembers complaining to her OB-GYN about the crying jags and sleep loss she was experiencing, but the doctor sent her home with suggestions of getting out of the house more. Jen dutifully tried that, then ended up “losing it” when her doctor asked how she was doing during a postpartum checkup. She was eventually diagnosed with postpartum anxiety – fun fact: postpartum disorders aren’t just relegated to depression – and was briefly hospitalized for observation. She began seeing a therapist and taking meds, and eventually her symptoms abated.
According to some studies, postpartum anxiety, which Jen had, may be even more common than straight PPD. On Parents.com, Jonathan Abramowitz, Ph.D., associate chairman of psychology and director of the Anxiety and Stress Disorders Clinic at The University of North Carolina at Chapel Hill, dubbed postpartum anxiety “the hidden disorder, because so few moms recognize it and it goes undiagnosed.” Its symptoms are similar to regular anxiety, but can grow even more severe—think racing thoughts, panic attacks, a powerful sense of dread, and sometimes, irrational baby-focused fears.
After she brought home her new son Eli, now-36-year-old Ket of Berkeley was diagnosed with postpartum psychosis, a more extreme sibling of the two. Postpartum psychosis is considered rare, occurring in just .1% of births; women with bipolar disorder or schizoaffective disorder are most at risk for developing it. But it can be frightening and quite serious, triggering delusions, hallucinations, paranoia, mania, mood swings, and difficulty communicating. According to Postpartum Support International, postpartum psychosis ends in suicide for approximately 5% of women afflicted, and there’s a 4% infanticide rate associated with it, too.
For her part, Ket had no history of mental illness, and she felt stunned by the onslaught of physical and emotional changes that hit her after she brought Eli home. Though she bonded with her son immediately, saying she was “obsessed with him,” she was also nauseous, unable to eat or sleep, constantly anxious, and she felt alone, despite the fact that her husband, friends, and family were there to help. “At the hospital, they prepare you for the birth, and then they send you home with your baby, like, ‘Everything will be great! You’ll be so happy,’” she remembers. “They don’t tell you it might be awful [at first].”
Ket began having panic attacks a few weeks later. She recalls being unable to determine when she was sleeping or awake, and after seeking help, she was diagnosed with postpartum anxiety, depression, and psychosis. Though her doctor wanted to put her on Zoloft, Ket resisted because she was breastfeeding. That is, she resisted until she had an episode so severe she couldn’t anymore. While her husband was away, Ket began having delusions. She started seeing spirits and believing her baby was the second coming of Christ; she also threw her contacts out the window while she was driving with the infant. She met up with a friend, who expressed profound concern, as did her husband when he returned. Seeking treatment, Ket was prescribed Zoloft and Zyprexa—an anti-psychotic medication—and this time she took them. Today she’s medication-free, and her family is healthy and happy.
When asked what cultural misconceptions bother her most when it comes to postpartum disorders like the ones she endured, Ket says, “You only hear about the depression. The anxiety and psychosis are considered [more extreme], and no one wants to talk about them. The best thing would be for more and more women to step forward and [admit] ‘I had this,’ not just ‘I was sad for a little bit.’”
Jen also believes women would benefit from hearing more stories like hers. Though she hasn’t told too many people about her postpartum anxiety, she notes, “When I do tell people, I’ve had so many new moms tell me that it [helped]. Part of the relief for some moms is knowing that it’s not bliss right away—that it’s OK to mourn your prior life.”
Follow us on Facebook, Instagram, and Pinterest for nonstop inspiration delivered fresh to your feed, every day.

