How to Tell If Your Nasty Cold Is Actually the Flu or COVID-19, According to Doctors

"Hearst Magazines and Yahoo may earn commission or revenue on some items through the links below."
This article was medically reviewed by Raj Dasgupta, M.D., an assistant professor of clinical medicine and a member of the Prevention Medical Review Board.
When you’re sick, all you care about is feeling less miserable—but once the temps drop during fall and winter, it can be tricky to figure out if you’re dealing with the flu, COVID-19, or a common cold.
So many of the symptoms overlap, but there are a few key differences to keep in mind. (More on that later.) Of course, in order to stop your sniffles, you need to know what’s causing them in the first place. Here, doctors explain how to figure out the answer to your pressing cold vs. flu vs. COVID-19 questions so you can seek the treatment that will actually make you feel better.
Cold vs. flu vs. COVID-19 symptoms
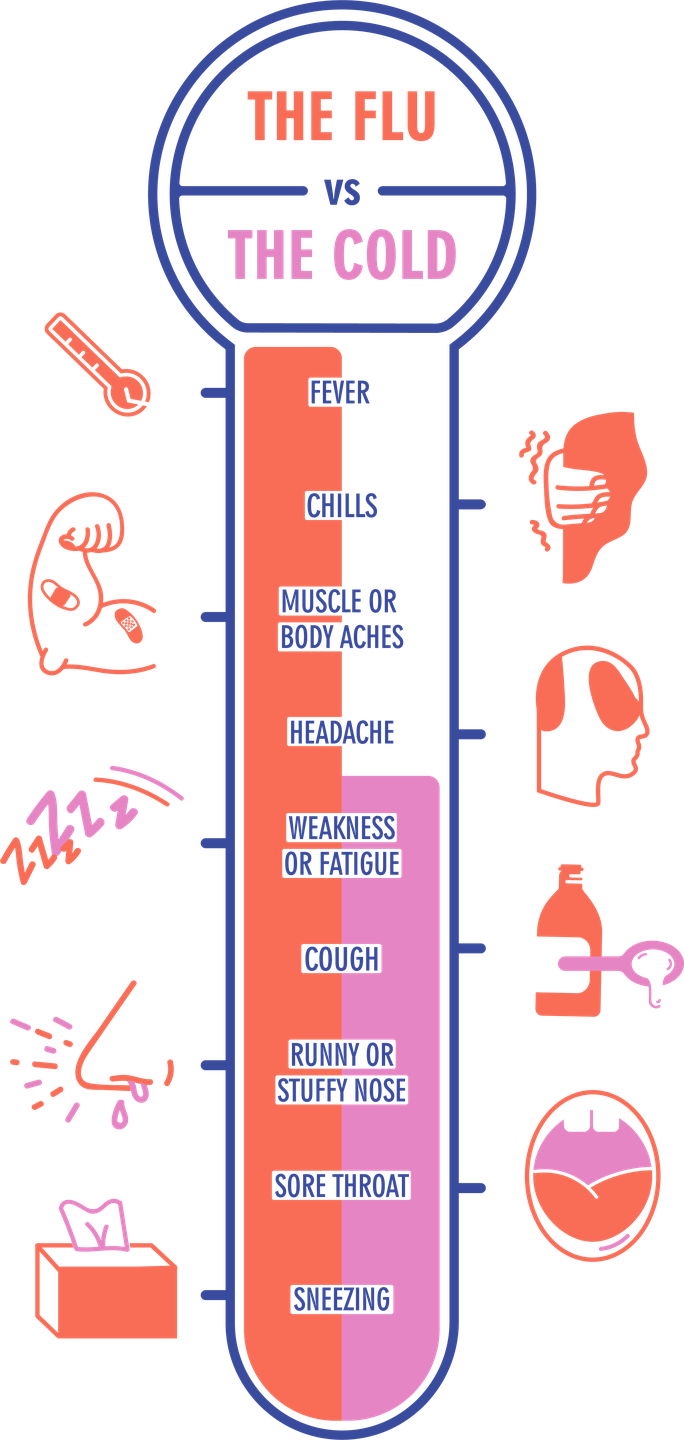
Part of the reason it can be tricky to know whether you have the flu or a cold or even COVID-19 is simply because there are only a few minor differences between their symptoms.
Cold symptoms
In general, cold symptoms show up primarily above your neck:
Coughing and sneezing
Slightly swollen glands
Minor aches and pains
Flu symptoms
This includes symptoms above and below your neck. You have all the signs of a cold, plus the following:
Fever over 100°F
Chest coughs
Weakness and fatigue
Headaches
Chills
Vomiting
Diarrhea
Full-body aches
And, again, because COVID-19 should be considered, too, here are the biggest signs of that illness, per the Centers for Disease Control and Prevention (CDC).
Fever or chills
Cough
Shortness of breath or difficulty breathing
Fatigue
Muscle or body aches
Headache
New loss of taste or smell
Sore throat
Congestion or runny nose
Nausea or vomiting
Diarrhea
How do I know if I have the flu or a cold?
The biggest differences between the symptoms of influenza and a cold are their severity and how quickly they develop. With the flu, “one day you are feeling OK, and the next, all your symptoms arise,” says Michael P. Angarone, D.O., professor of infectious diseases at Northwestern Memorial Hospital.
Compared to the flu, a cold is milder and symptoms gradually set in. “The flu is like a cold on steroids,” says Joseph Ladapo, M.D., Ph.D., professor of medicine at the University of California, Los Angeles. “I’ve heard patients say, ‘This is worst I’ve ever felt in my life.’”
He also adds this: “If you don’t feel horrible, you probably don’t have flu.”
But, like many illnesses, it’s tricky to say that this will happen in every situation. “You can be walking around with the flu—there are all different levels of severity,” says Timothy Murphy, M.D., senior associate dean for clinical and translational research at the University at Buffalo Jacobs School of Medicine.
Infectious disease expert Amesh A. Adalja, M.D., a senior scholar at the Johns Hopkins Center for Health Security, agrees. “It’s impossible to really differentiate a cold from influenza because the symptoms overlap,” he says. “Influenza tends to be more severe and associated with fever and muscle aches, but it could be mild enough to be confused with the common cold.”
It also matters if you’ve been vaccinated against the flu. While the flu vaccine won’t necessarily keep you from getting sick—vaccine effectiveness has ranged from 19% to 60% over the past decade, per CDC data—it “can give partial protection and can turn what would have been a more severe illness into a minor illness,” Dr. Murphy says.
David Cennimo, M.D., assistant professor of medicine-pediatrics infectious disease at Rutgers New Jersey Medical School, agrees. “People who get vaccinated against influenza and have a ‘breakthrough’ infection tend to be much less sick with more mid symptoms that can be confused with a cold,” he says. “This confusion means that we really do need testing to be sure.”
Basically, it can be confusing, even when you know all the classic signs of each illness. Still not sure what’s happening with your health? Asking yourself these question can help:
How severe does this feel?
Cold: You feel mildly icky, and things get worse slowly. The first signs might include slight aches, a scratchy throat, a headache, and/or a low-grade fever.
Flu: The flu usually hits you like a speeding train. You may first feel feverish at work, and by the time you get home you can barely muster enough energy to climb your porch steps. Every inch of you aches.
Can I get out of bed?
Cold: Yes, you can walk around. Though you might not want to commute to work or schlep the kids around, you can manage.
Flu: In many cases, you’re flat on your back. Extreme fatigue may incapacitate you for at least a few days.
What to do if you develop symptoms
In the past, doctors would usually recommend that you see your doctor if you have cold- or flu-like symptoms that make you feel lousy. But with COVID-19 now in the mix, that advice has changed a little. “Do not to go right to your healthcare provider,” says William Schaffner, M.D., an infectious disease specialist and professor at the Vanderbilt University School of Medicine.
“Any respiratory symptoms…should prompt COVID testing,” Dr. Adalja says. If that’s negative and you think there’s even a chance you could have the flu, Dr. Adalja recommends calling your doctor about getting tested for the flu. “There should be a low threshold for influenza testing because there are influenza antivirals that people can benefit from—if given early enough—especially the high risk,” he says.
Should you wear a mask if you’re sick?
The rules of navigating an illness have changed thanks to the pandemic, and it’s now generally considered courteous to wear a mask if you’re sick. This isn’t just an etiquette thing—it can actually help keep your illness from spreading, Dr. Adalja says.
“If people are sick with any respiratory virus and can’t isolate or social distance, they should wear a mask in order to decrease transmission to others, especially indoors,” Dr. Adalja says.
Cold vs. flu vs. COVID-19 treatment
If you aren’t sure what you have and how to treat it, talk to your healthcare provider over the phone or make an appointment to see them in person, Dr. Angarone recommends.
Cold treatment
Take it easy and rest up. Keep a water bottle nearby to ensure you’re staying hydrated. Popping a pain reliever like ibuprofen or acetaminophen may temporarily perk you up.
A cold can follow you around for as long as 10 days, but you don’t have to quarantine yourself the entire time. Once you start feeling better, you’re no longer very contagious, so you can head back to work as long as you’re up for it.
Flu treatment
Plan to hunker down for three to seven days, and ask your MD about Tamiflu. “If taken within 48 hours, it will help you get better sooner and reduce the chance that you’ll pass the virus to others,” says William Schaffner, M.D., an infectious disease specialist and professor at the Vanderbilt University School of Medicine. You can go back to normal life 24 hours after your fever recedes on its own, but you’ll probably be moving slowly for a bit.
COVID-19 treatment
Check in with your doctor to see if you’re considered high risk for severe complications of COVID-19 and a candidate for an anti-viral medication like Paxlovid, Dr. Schaffner says. (This checklist can help.)
If your illness is mild, you can treat your symptoms at home with over-the-counter medications like acetaminophen (Tylenol) or ibuprofen (Motrin, Advil), the CDC says.
You should plan to stay in isolation for at least five days from the time your symptoms started, per CDC recommendations. You can end your isolation after five days if you were symptom-free or if you’ve been fever-free for 24 hours without the use of fever-relieving medication, the CDC says. Regardless, you should also wear a mask when you’re indoors and around others until day 11.
When to see a doctor about your cold, flu, or COVID-19 symptoms
Call your doctor if you experience:
Symptoms that overlap with signs of COVID-19
Trouble breathing or eating (call ASAP)
You have a fever higher than 100.4°F
You’re experiencing severe vomiting or diarrhea
Coughing lasts longer than 10 days, is driving you crazy, or is making it hard to sleep
Upper-respiratory symptoms last more than a week or 10 days
How to lower your risk of getting sick in the first place
Viral illnesses happen. But doing your best to take the right precautions can lower the risk you’ll have a miserable week or two this winter, Murphy says. That’s why he recommends getting your annual flu shot, along with your COVID-19 vaccine (and your booster shot, if the timing is right.)
Otherwise, Dr. Schaffner suggests following COVID-19 prevention strategies most people have memorized over the past two years. “Wash your hands, wear your mask in public, and avoid people who are coughing and sneezing,” Dr. Schaffner says. “Those mitigation strategies really reduced influenza in this country last year and even cases of the common cold—they will continue to help this year.”
You Might Also Like

