Can You Find Out What Strain of COVID-19 You Have? It's Trickier Than You Think
The Omicron variant of COVID-19 has quickly taken over as the dominant strain of the virus in the United States. Omicron, which was responsible for just 0.7% of COVID-19 cases in the country on December 4, was responsible for a whopping 73.2% of cases on December 18—and that percentage is expected to grow.
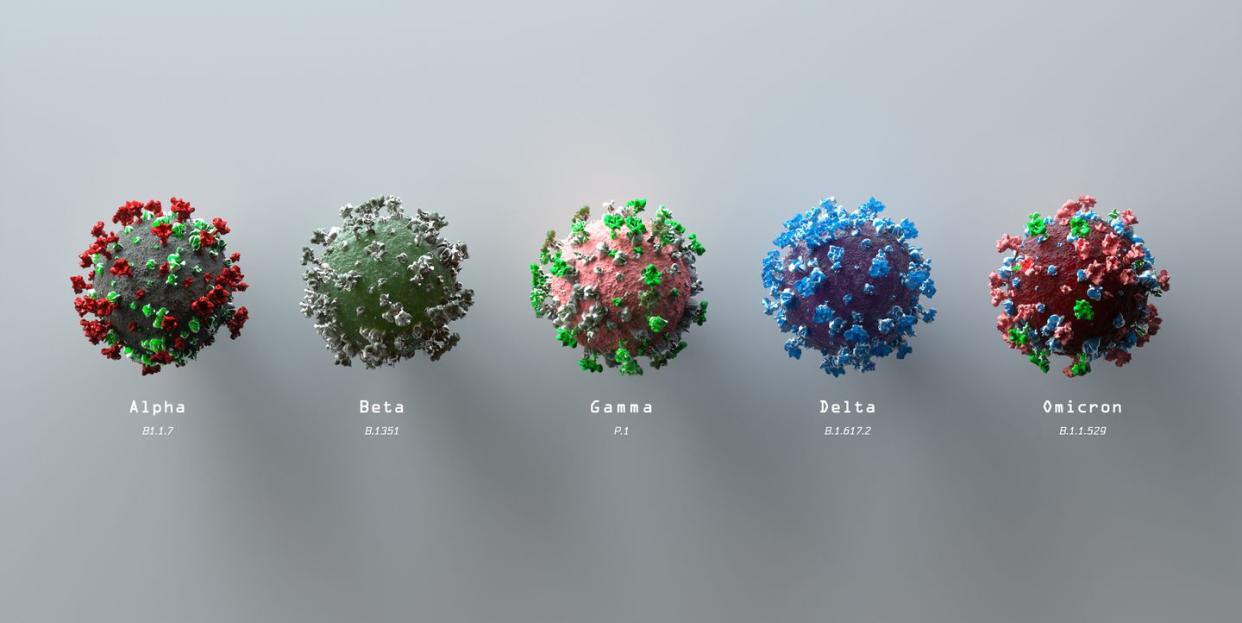
With this, Omicron has unseated the Delta variant as the dominant strain of SARS-CoV-2, the virus that causes COVID-19, in the country. If you’re diagnosed with COVID-19, it’s more than understandable to want to know what strain of COVID you have. While doctors say this isn’t easy information to obtain—even for them—there may be a way to learn what strain of COVID-19 you have. Here’s what you need to know about how to know what strain of COVID you have.
How do public health officials know what strains of COVID people have?
When the Centers for Disease Control and Prevention (CDC) releases information on percentages of variants in the U.S., they’re not analyzing every single positive test in the country to get those numbers, explains Thomas Russo, M.D., professor and chief of infectious disease at the University at Buffalo in New York.
Instead, the CDC conducts genetic sequencing on a percentage of positive tests across the country. For example, to get the latest results, the CDC analyzed 160 test results from Alabama, 4,157 from Arizona, 18,424 from California, and so on, to get a breakdown of what percentage of those positive tests matched up with a particular strain of COVID-19.
CDC officials and lab technicians don’t even know whose test results they’re analyzing—for privacy purposes, they’re de-identified before testing. Meaning, your name is taken out of the equation. As a result, the CDC couldn’t call you or your doctor and say what strain of COVID-19 you had, even if they had the manpower to do it, Dr. Russo points out.
Does your doctor know what strain of COVID you have?
Not usually, and there are a few reasons for this. “The tests that are run by doctors in offices and hospitals don’t sequence and specify the variant,” says infectious disease expert Amesh A. Adalja, M.D., a senior scholar at the Johns Hopkins Center for Health Security. The rapid antigen tests that are often used to get quick results instead just tell if the test result is positive or negative for COVID-19.
Even a PCR test, which is considered the gold standard of COVID-19 testing, “is not going to tell you—it’s not going to sequence the test,” Dr. Adalja says. PCR testing can also take days to give you results, which is why your doctor will typically just do a rapid test in their office to help you know quickly whether you have COVID-19 or not, Dr. Russo explains.
OK, so is there any way to find out what strain of COVID you have?
Here’s where things get a little tricky. The Omicron variant has a particular genetic sequencing that can show up differently on PCR test results that you wouldn’t see with other strains of COVID-19, like Delta. It’s called S-gene target failure and can show up as a “band drop-out” on the test results, Dr. Russo says.
“This can give you a hint that it’s Omicron, but it’s not definitive,” Dr. Adalja says. “Right now, if you got a PCR test, the lab technician could tell you that this looks consistent with Omicron.”
That said, Dr. Adalja points out that most family medicine doctors aren’t going to be asking about this—they typically just want to know if you're positive or negative. It’s more something that infectious disease experts and microbiologists would ask about. Still, he says, “If you wanted to know and your doctor gave you a PCR test, you could ask them if there was S-gene target failure. If there is, for all intents and purposes, that’s an Omicron.”
There’s a slight caveat with all of this, though: Dr. Russo points out that not every case of Omicron shows up with S-gene target failure on a PCR test result. “We’re still trying to understand why that is,” he says. So, it’s possible to have Omicron and not have that show up on a PCR test result—or you could simply be infected with the Delta strain.
Can your symptoms tell you what strain of COVID you have?
It won’t be a slam-dunk diagnosis, but there may be some indication if you have one variant or the other, depending on your COVID-19 symptoms and vaccination status, Dr. Russo says.
If you’re fully vaccinated, it’s been at least two weeks since you’ve had a booster shot, and you still contract COVID-19, the odds are high that you have the Omicron variant, Dr. Russo says. “Statistically speaking, you’re more likely to be infected with Omicron than Delta anyway,” he says. “But that’s particularly true if you’ve been boosted—Omicron seems to be more resistant to vaccination.”
According to a recent CDC study, those symptoms may include:
Cough
Fatigue
Congestion
Runny nose
But if you haven’t been vaccinated against COVID-19, Omicron and Delta are likely to cause similar symptoms of COVID-19. Per the CDC, those include:
Fever or chills
Cough
Shortness of breath or difficulty breathing
Fatigue
Muscle or body aches
Headache
New loss of taste or smell
Sore throat
Congestion or runny nose
Nausea or vomiting
Diarrhea
How much does knowing the strain of COVID you have matter?
For the average-risk patient, it doesn’t really matter, Dr. Russo says. “At the end of the day, if you’re infected, you want to go ahead and monitor for more serious symptoms like shortness of breath and present to your healthcare provider, regardless of if you’re infected with Delta or Omicron,” he says. “For healthcare providers, symptoms and severity of illness usually drive treatment.”
There is one exception, though. “Certain monoclonal antibody treatments don’t work against Omicron,” Dr. Adalja says. He specifically cites the Eli Lilly monoclonal antibodies as being expected to be less effective against the variant, while GSK’s monoclonal antibody treatment is expected to do well against Omicron. “It’s important from a clinical perspective for someone who is high risk to know that information,” Dr. Adalja says.
Still, “getting that information within the needed timeframe may be challenging unless the diagnosis was via PCR and S-gene target failure occurred and that information was readily available to the provider,” Dr. Russo says. Basically, there are a lot of “ifs” involved. Given that Omicron is now the dominant strain of COVID-19, Dr. Adalja says that resources are likely to shift to allow for more production of GSK's monoclonal antibody treatment, just to be safe.
Overall, doctors say it’s not vital for you or most other COVID-19 patients to know what strain of the virus you have. However, it doesn’t hurt to ask.
You Might Also Like

