I Lost My Son to a Rare Cancer. I Don't Want Others to Go Through the Same Pain.

When my son Finn was diagnosed with a rare form of cancer in 2016, my husband and I were ready to fight. That’s when we realized—after watching our son go through several intense, painful, and ultimately unsuccessful primary treatment plans, all before he was too old to tell us how or what he was feeling—that doctors don’t always have the answers. The truth is, the healthcare industry is set up to fail too many patients, our Finn included. I’m sharing our story in the hopes that future families won’t have to experience the same uncertainty and helplessness we did while fighting for our son’s life.
To me, there’s nothing better than being a mom, even as tragic as my journey in motherhood has been. I love kids and have always wanted to raise them. So when I met my now-husband Dan during our junior year at Syracuse University and we decided to get married in May 2006, starting a family was high on my priority list.

"Did I Give Him Something to Cause the Cancer?"
Finn was our third baby. Gavin, our first, was born in 2009, followed by Everett in 2012. Finn came along almost exactly two years after Everett, and he was healthy from the get-go.
In wanting to give my kids the best start in life that I could, I nursed all three of them. I also made sure to feed them whole foods because I’d done a lot of research on the importance of feeding your kids a healthy diet from early on. So you can imagine, I was pretty shocked when Finn was diagnosed with cancer at the age of one and a half.
Finn had a very rare form of cancer called embryonal rhabdomyosarcoma. The cause of rhabdomyosarcoma is still not known, but I now know it’s likely caused by genetic or familial inheritances and not caused by anything environmental. But as a parent, you tend to beat yourself up. Did I eat something while pregnant that caused the cancer? Did I give him something? I find myself going back to those early years of Finn’s life and thinking Dang, I did everything I knew to do. You do your best to give your kids all the right things from the start, and then they still end up with cancer. You never see it coming.
When Finn first got sick we had just moved from upstate New York to the Nashville suburb of Franklin, Tennessee. He’d had a bout of pneumonia that winter, but otherwise had been a healthy child. So when he came down with a common cold in July, I didn’t think much of it at first. We’d been visiting different churches, and I assumed he’d picked something up in a nursery. But then it quickly turned into a second case of pneumonia, which was extremely odd for a child to have within six months and put me on alert. Then he started showing signs of constipation, but after-hours clinic doctors said it was probably a side effect of his pneumonia treatment.

This went on for about three weeks, which is agonizing to think about now. It’s not unusual for people ultimately diagnosed with a rare cancer to receive an initial misdiagnosis. We now know what was actually happening is that a tumor was growing inside of his bladder. But no one did scans or tests to see if the constipation was something more until I found a pediatrician in early August. Even then, she ordered an x-ray of Finn’s abdomen and it did appear his bowels were backed up, but no further testing was done. A few days later Dan and I noticed blood in his urine.
Since Finn was young and didn’t yet have the language skills to tell us what was hurting, I had to act like a detective and study his body for signs to figure out what was wrong. Gavin is non-verbal, so I was used to this. But it’s still heartbreaking to watch your child in pain and have no idea how you can take it away. That’s why I was actually relieved when I saw blood in his urine. I thought it meant a UTI or some other blockage that we could treat.
The pediatrician ran some tests and referred us to a urologist, but we never made it to that appointment. The next morning when we woke up, I noticed a golf ball-sized bulge on the right side of Finn’s abdomen. I started to panic. I took a picture and texted it to my husband and told him I was taking Finn to the ER.
Trusting My Instincts
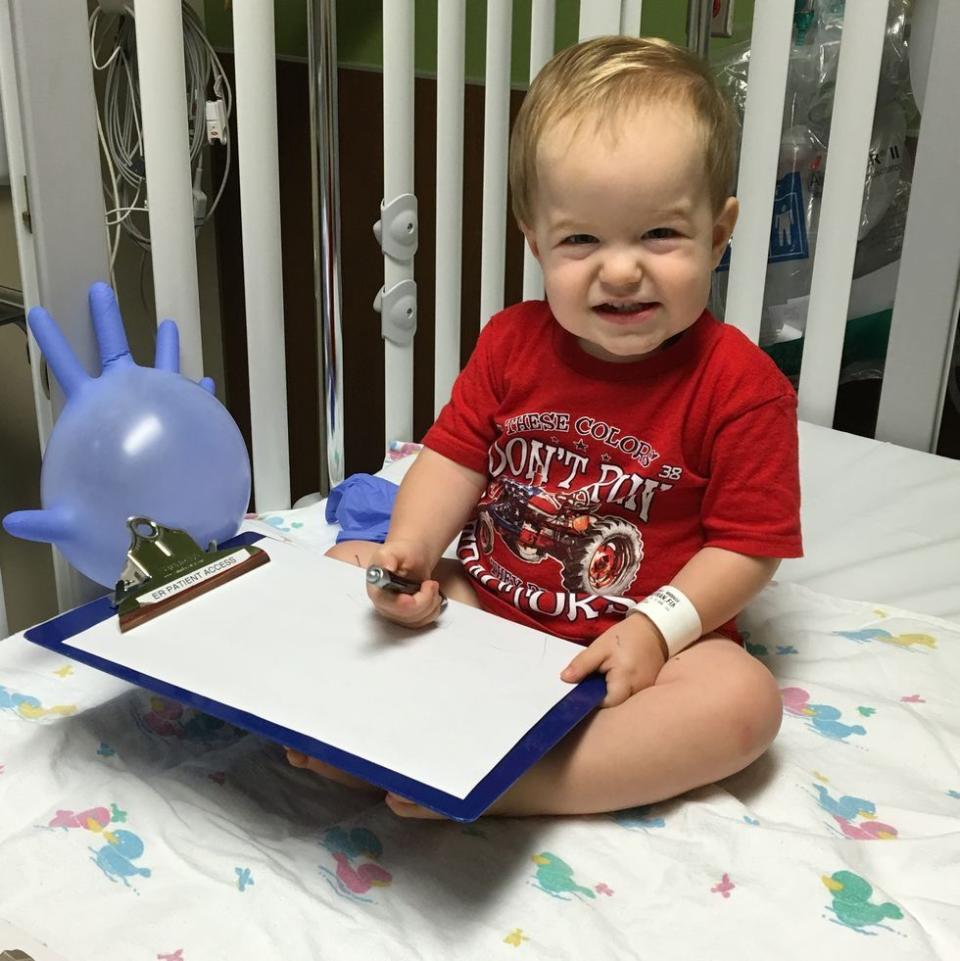
By some miracle, no one else was in the ER when we arrived that morning. So it was quiet and all of the attention was on Finn. They did an ultrasound and found a mass in his bladder. The doctor didn’t even wait for the radiologist to read it. When her tech showed it to her, she came to see me right away. She said she didn’t know what it was, but that we needed to go to Vanderbilt Children’s Hospital that day.
Our pastor’s wife drove Finn and me over there while my husband arranged for childcare for Gavin and Everett before meeting us at Vanderbilt. There, doctors did a more in-depth ultrasound and they didn’t even wait for a biopsy—the oncology team came to talk to us that day to tell us they believed it was one of two things. There are very few things inside of a child’s bladder, so I think they knew pretty quickly that it was a rhabdomyosarcoma tumor. That was Tuesday, August 16, 2016. A parent never forgets the date when she learns her child’s life is at stake.
The week that followed was a whirlwind of scans, biopsies, and starting chemotherapy. By the time doctors had discovered Finn’s tumor, it was already stage three. Unfortunately, that’s typical of RMS because it grows very quickly. We went from a normal Monday morning, to a cancer diagnosis, to putting a port in and starting chemo within the span of five days. His treatment plan required 43 weeks of chemotherapy, 28 days of radiation, and was scheduled to take 10 months.
I remember the terrible traffic driving to the hospital every day. Finn screaming and crying in the car because he was in so much pain, and hungry because they had to sedate him for the radiation and he couldn’t eat before. I remember needing to give him Oxycodone to sleep because otherwise the pain kept him up all night. There were so many days when all I could do was hold him while he cried.
But you have your game face on and you just go, go, go because you have to. Dan and I really relied on each other and God to get through it. And luckily, we had our neighbors and church who all stepped up to be there for our family. We also had family take turns coming down from New York to stay with us to help through Finn’s treatment.
As hard as Finn’s treatment was, I think we were all pretty hopeful. The doctors did scans throughout the chemo regimen and the first one was at nine weeks—Finn’s tumor had already shrunk by 50 percent. With rare cancers like Finn’s, you never know if the treatment is going to work. So we were so excited when we got that news. But what they don’t always tell you is that a shrinking tumor doesn’t necessarily mean anything. You can kill off some of the cells, but that doesn’t mean that what I call the “Mother Cells” are going to die off as well.
Finn finished treatment at the end of June 2017. His final scans showed there was still a residual mass in his bladder, which the doctors had warned us could happen. My Mom Instincts were telling me it wasn’t a good thing, but doctors assured us the tumor responded to the chemo and radiation as well as could be expected and suggested the mass could just be scar tissue. The only thing to do was monitor it.
We’d planned a week-long trip to New York to visit our families and celebrate the end of Finn’s treatment three weeks after he finished chemo. That’s just when the strongest elements of the chemo start to leave your system. I was devastated, but not entirely surprised given his last scans when, halfway through our trip, Finn started experiencing the same symptoms he’d had when he was first diagnosed.
We scheduled an ultrasound as soon as we got back to Nashville. And to me, the mass in Finn’s bladder looked bigger. Our urologist didn’t think it had grown, but agreed we needed to monitor Finn. This is where I always advocate to parents, if your instincts are telling you something is wrong with your child, don’t doubt yourself. You know your child best. I told the doctor at that appointment: “I’m sorry but I’m going to nicely disagree with you. I’ve stared at that thing for the last year and watched it shrink and studied it and I know it’s bigger.”
At this point, we had some difficult choices to make. When the urologist looked at Finn's bladder through the scope in July during a catheter procedure to relieve Finn’s pain (from what we suspected was the tumor growing), he said it looked like the bladder of a 70-year-old man with prostate issues and we needed to consider removing his bladder regardless of the tumor growing. Finn had a scheduled scan in August as a follow up to his original treatment plan. Sure enough, at that scan they measured the mass and it had indeed grown. The cancer was still alive. We scheduled surgery for September 11 and requested one more scan to be sure it was still growing. Once we knew from the second scan that the tumor was in fact growing, we moved ahead with surgery to remove his bladder and prostate and Finn started two relapse chemos in November. But when we went in for his first scheduled scan in February, the urologist and oncologist called me over after a day in clinic for chemo and told me a new tumor had grown in Finn’s pelvis while he was on the relapse chemo regimen.
Dan and I wanted to keep fighting, but our doctors told us, “The target for a cure for Finn may still be out there, but it is getting very small and we don’t know what that is.” That wasn’t good enough for us, so we decided to seek a second opinion.
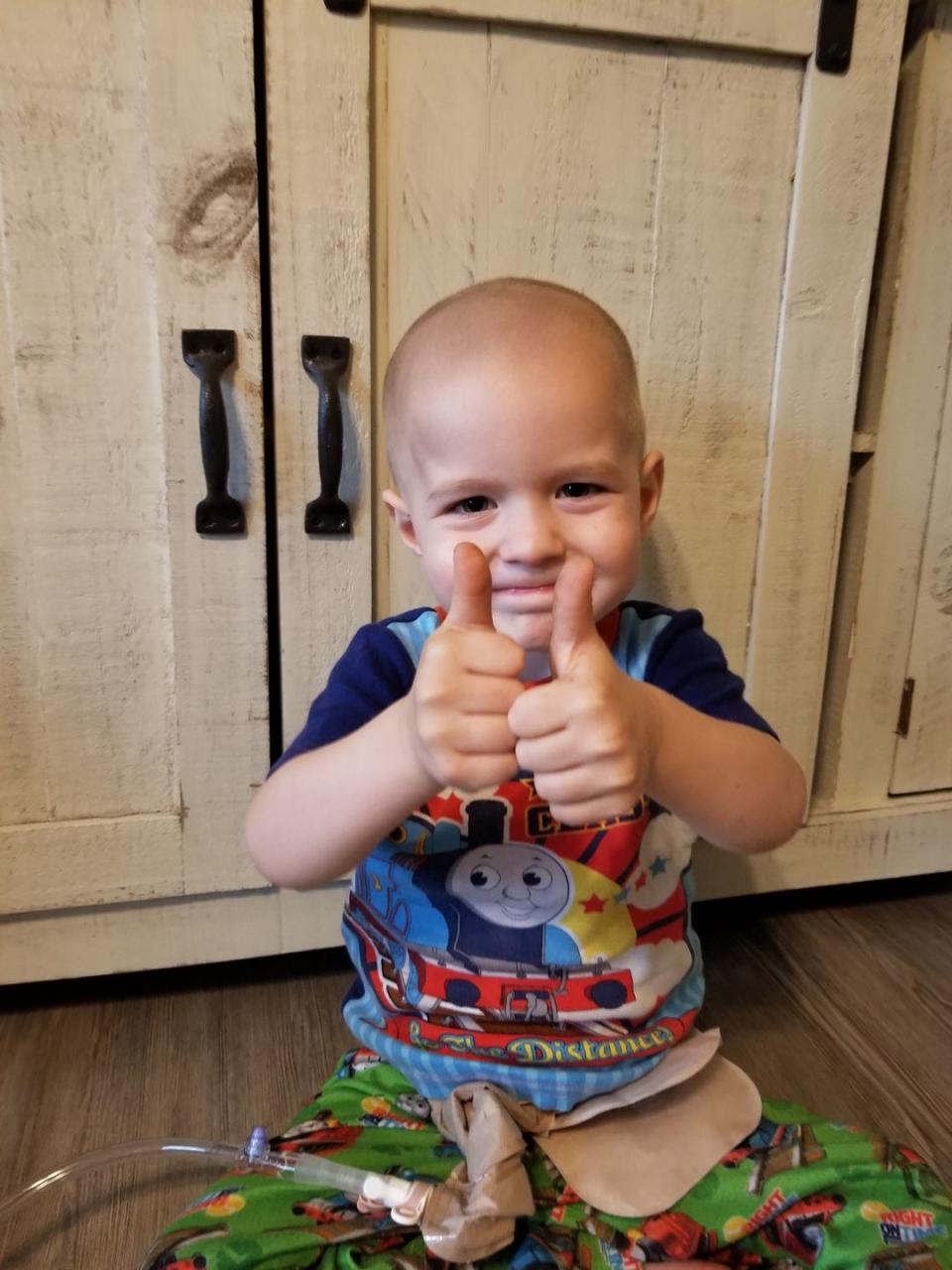
Our urologist put us in touch with a urologist at Duke University Medical Center who told us to talk to Carola Arndt at the Mayo Clinic in Rochester, Minnesota. She has been an oncologist for decades and is a leading expert on RMS. So if anyone was going to know how to help Finn, it was her. It was there at Mayo, after meeting two pediatric urologists who led Finn’s case that we found new hope. The amazing sarcoma team at Mayo did scans and even built a 3-D model of Finn’s tumor to show us what they planned to do during surgery that March. It was intense and ended up being two surgeries in the course of four days. Doctors had to take Finn’s rectum, front pubic bone, a bunch of tissue, a nerve, and part of a muscle to get clean margins. We followed that up with another more intense relapse chemo regimen that consisted of four- and five-day stays in the hospital. He was supposed to receive six cycles of that chemo regimen, but we had to end it after only three because the large incision down his abdomen and pelvis that had been used for four surgeries was not healing while Finn was on chemo. He looked to be in the clear after the first scan in August post the three chemo cycles, but a month later Finn’s scheduled scan showed two new tumors had grown again. Desperate at this point, we went back to Mayo Clinic to evaluate what our options were. We determined that radiation for one week and then surgery was our best option. Surgery was scheduled in October, but just a few hours into that final surgery, the doctors called and said they couldn’t move forward. They’d found tiny microscopic tumor seeds all throughout Finn’s abdomen and surgery wouldn’t help. The cancer had spread everywhere. We were completely devastated. I remember just crumbling to the ground and Dan holding me.
Forever Changed
We flew home to Nashville with Finn on the private medical Mayo Clinic jet, spent one night at Vanderbilt, were discharged from the hospital on October 31, 2018, and moved to hospice care at home. Even then, I wasn’t willing to give up all hope. Our doctors at the Mayo Clinic helped identify a couple palliative chemotherapies in pill form to try for a “Hail Mary.” And we were continuing other holistic options we were given with the help of a cancer coach.
Around this time I got in touch with David Hysong, founder of Shepherd Therapeutics, the first pharmaceutical and biotech company aimed at curing rare cancers like RMS. He started the company after being diagnosed with a rare head and neck cancer known as adenoid cystic carcinoma in 2015. Like Finn, the treatment options he’d been given were pretty bleak; doctors told him he had between five and 10 years to live. But rather than accept that, David decided to fight—for himself and for hundreds of thousands of people who are diagnosed with rare cancers every year.
When Finn moved to hospice care, I called him up and told him, “I know I’m just a parent, I’m not a scientist. But whatever happens with Finn, I’m forever changed and I need to help you make a difference.”
I didn’t know it at the time, but David had been struggling himself. He was in Dubai and facing a lot of opposition from potential investors and others in the healthcare industry who told him his plans for Shepherd would never work. “Shepherd shouldn’t be a company,” he remembers them saying. Later, he told me my call is what encouraged him to keep going, reminding him of the lives that would never be saved if Shepherd failed.
In Finn’s final days, it was moving to see how our community continued to rally behind our family. We’re members at the local Elk’s Lodge, and they brought an early Christmas to Finn by throwing a big holiday party in our cul-de-sac with a Santa and hot cocoa. That was really special. A local church even helped out by bringing Christmas gifts and donating two Christmas trees decorated for Finn. One was superhero themed, the other was all green and had avocado ornaments on it. It was deeply humbling to have so many people love our family and give Finn one last time the thing every child yearns for: Christmas.

Avocados were Finn’s favorite food. During treatment, he had phases when he couldn’t eat solid food and an avocado was always the first thing he asked for once he was able. My husband filmed this adorable video of him eating one in the hospital that he posted to Facebook. In it, Finn is just smacking his lips like he’s really enjoying the avocado—talk about melt your heart!
We were hopeful until the last moment, and all along it was hard not to do the ‘what if’ spiral. What if I hadn’t slept and stayed up all night and found a clinical trial that could have been the answer? But I know that’s not productive. What is productive is sharing Finn’s story and helping bring awareness to RMS and the other rare cancers. In the early morning hours of December 2, 2018, Finn passed away in our arms.
All of this is possible if we add our voices and demand these changes. Please join me and David and share your concerns about rare cancer with Congress by going here and entering your zip code to send a message directly to your Member of Congress. You can tell them we must address rare cancer through molecular diagnostics of all cancer subtypes and more investment in research and development for rare cancer therapeutics. Molecular diagnostics for every distinct cancer subtype would make a huge difference in understanding not just my son’s cancer, but all forms of cancer. With this understanding, physicians can improve care and researchers can advance more targeted therapeutics to address the drivers of these cancers. And if you can, please donate here. Your contribution will strengthen Shepherd patient advocacy and research efforts to help save lives.
Our motto is “If not us, then who?” Because all of us deserves a fighting chance.
Stay updated on the latest science-backed health, fitness, and nutrition news by signing up for the Prevention.com newsletter here. For added fun, follow us on Instagram.
You Might Also Like

