What to Know About Babesiosis, the Rare Tick-Borne Illness That Attacks Red Blood Cells
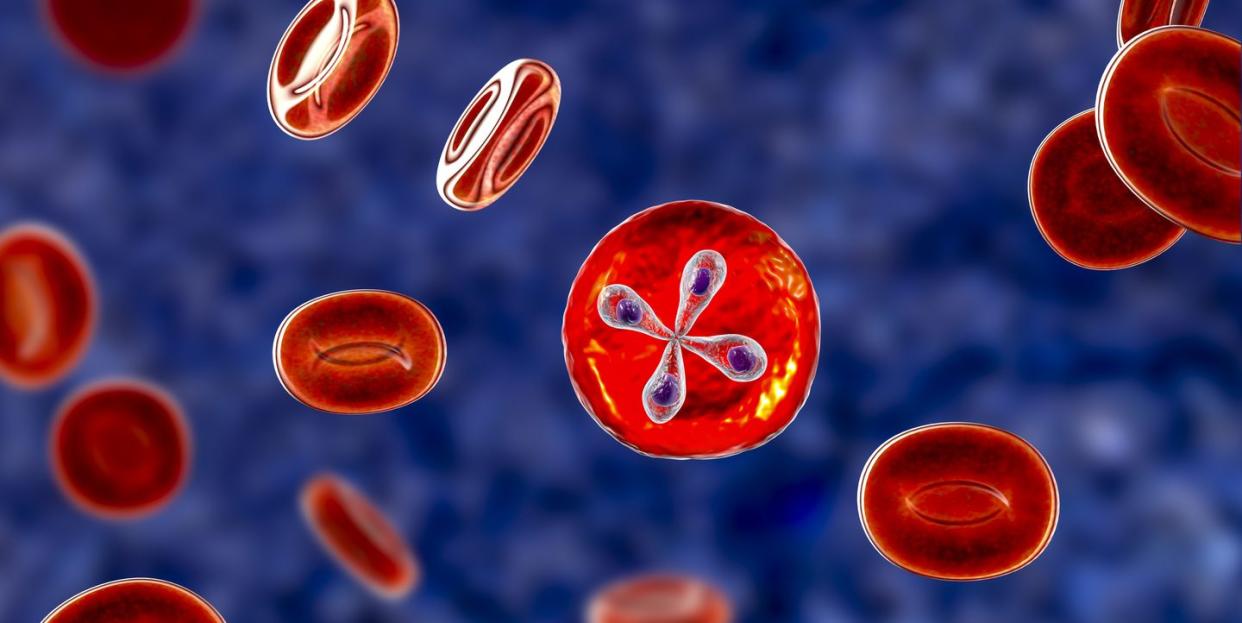
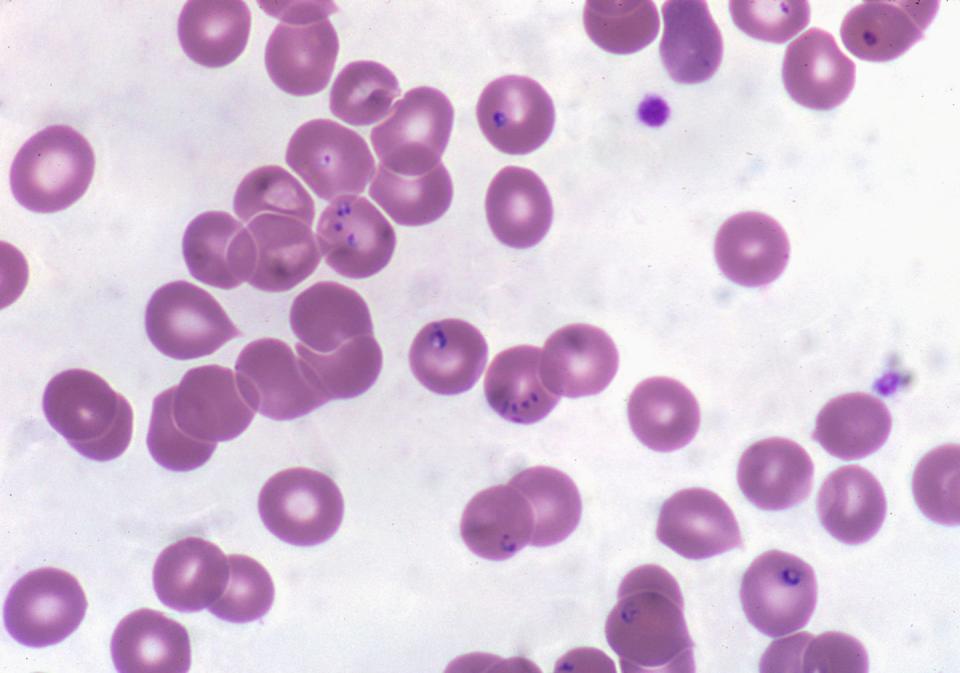
You’ve already heard about the devastating effects of Lyme disease, the most common tick-borne illness in the U.S. But there are others to have on your radar as the tick population booms this summer, including babesiosis, a disease that’s caused by microscopic parasites that infect the red blood cells, according to the Centers for Disease Control and Prevention (CDC).
In a recent report, The Washington Post spoke to the family of Jeff Naticchia, 51, who started experiencing mysterious symptoms that eventually landed him in the emergency room. He was misdiagnosed with a kidney infection and only briefly felt better with antibiotics before his symptoms worsened. He couldn’t breathe well and the whites of his eyes turned yellow, forcing his doctors to move him to an intensive care unit, where he was placed on a ventilator.
Finally, an infectious disease doctor came back with a new diagnosis: babesiosis. Suddenly, things made sense. Naticchia recalled removing a super-tiny tick from his body that summer.
Babesiosis is spread by the same tick that causes Lyme disease and can have odd symptoms that can be confused with other illnesses, making it difficult to diagnose. What’s more, reported case counts of babesiosis are estimated to be much lower than they truly are. Here’s what you should know about babesiosis and how to stay safe this summer.
Back up: What causes babesiosis?
People mainly contract babesiosis through the bite of a blacklegged or deer tick that is infected with Babesia microti, parasites that often infect small mammals like white-footed mice. The disease is usually spread by tick nymphs (i.e. immature ticks) that are about the size of a poppyseed, the CDC says. These tick nymphs are typically most active during the warmer months in wooded, brushy, or grassy areas.
It’s also possible—but not very common—to get babesiosis from receiving a contaminated blood transfusion, as there are no tests for donor screening, per the CDC. Babesiosis can also be spread from an infected mother to her baby during pregnancy or delivery.
What are the symptoms of babesiosis?
Some people who are infected have no symptoms, but others can develop the following, according to the CDC:
Fever
Chills
Sweats
Headache
Body aches
Loss of appetite
Nausea
Fatigue
Babesiosis can also cause hemolytic anemia, which is the destruction of red blood cells. According to the National Heart, Lung, and Blood Institute, those symptoms can include:
Fatigue
Dizziness
Heart palpitations
Pale skin
Headache
Confusion
Jaundice
A spleen or liver that’s larger than normal
Pain the back and abdomen
Chills
Fever
Symptoms can start within a week, but can also take months to show up.
Where do most babesiosis cases happen?
“In parts of our country where one would contract Lyme disease, you can also contract babesiosis,” says Thomas Russo, M.D., professor and chief of infectious disease at the University at Buffalo in New York.
Most cases of babesiosis happen in the Northeast and upper Midwest, including New England, New York state, New Jersey, Wisconsin, and Minnesota, per the CDC. In addition to inland locations, babesiosis can be contracted in coastal areas, including Nantucket and Martha’s Vineyard in Massachusetts, Block Island in Rhode Island, and Shelter Island, Fire Island, and eastern Long Island in New York.
How common is babesiosis?
Data from the CDC show that there are around 2,000 babesiosis infections reported each year. In 2018, which is the most recent year that data is available, there were 2,161 reported infections.
“That’s likely an undercount,” says infectious disease expert Amesh A. Adalja, M.D., senior scholar at the Johns Hopkins Center for Health Security. He points to research that has found 7% of the general population in Nantucket has antibodies to Babesia as evidence. CDC data listed 527 babesiosis infections in all of Massachusetts in 2018, which would be less than 5% of Nantucket’s population.
Babesiosis can also overlap with Lyme disease because it’s transmitted by the same tick, Dr. Adalja explains. So, yes, you could be bitten by a tick that gives you both Lyme disease and babesiosis at once. If your doctor tests you for babesiosis, you can be accurately diagnosed. But if they just test you for Lyme—or something else entirely—it’s possible to miss the diagnosis.
However, babesiosis appears to be “less common than Lyme disease,” Dr. Russo says. By comparison, about 30,000 cases of Lyme disease are reported to the CDC each year—but experts estimate that number is closer to 476,000, due to unreported cases. Researchers are still trying to figure out if a Lyme-babesiosis coinfection is common, as much of the available data was collected over a decade ago.
How is babesiosis treated?
Babesiosis is diagnosed with a blood test. If you test positive, your doctor will likely give you the antifungal and anti-parasitic medication atovaquone, along with the antibiotic azithromycin, Dr. Russo says. That’s true even if your diagnosis just happens to be randomly picked up during other blood work and you don’t have symptoms. “You just don’t know what the potential consequences would be down the line,” Dr. Russo says, so it’s important to treat the infection as soon as possible.
In severe cases, patients will be given the antibiotic clindamycin and anti-parasitic medication quinine, the CDC says. These medications help fight the Babesia microti infection and clear the bacterial infection that can happen as a result of babesiosis.
Do people recover from babesiosis?
“Most people recover from babesiosis, but about half who get it will be hospitalized,” Dr. Adalja says. There are certain people who are at a higher risk of having a severe, life-threatening form of babesiosis, including people without a spleen, people who are immunocompromised, people with serious health conditions like liver or kidney disease, and elderly people.
For people who fall into the high-risk category, “mortality can be high,” Dr. Adalja says, as their immune systems just aren’t as well equipped to fight the infection.
How to protect yourself from babesiosis
If you live in an area where babesiosis or other tick-borne illnesses are more common, Dr. Adalja recommends amping up your tick bite prevention efforts, especially during the summer:
✔️ Be aware of your surroundings: It’s a good idea to avoid wooded and brushy areas with high grass and leaf litter. Walk in the center of trails when possible.
✔️ Wear a strong tick repellent or treat your clothing and gear with a permethrin-based product.
✔️ Closely examine yourself for ticks as soon as you get home by doing a full-body check around your underarms, ears, belly button, knees, waist, hair, and groin.
✔️ Shower within two hours of coming home from being outdoors.
✔️ Wash your clothing with hot water after being outdoors to ensure any lingering ticks are killed or tumble dry them on high heat for at least 10 minutes.
If you do get a tick bite, read this guide on how to remove it properly. Then, Dr. Adalja recommends keeping an eye out for any unusual symptoms within the next month or so. If you happen to develop any, call your doctor and let them know you’ve been recently bitten by a tick. They should be able to treat you appropriately from there.
You Might Also Like

