Five breakthroughs pushing us closer to a cure for cancer
Last month, news broke of an experimental drug that could “annihilate” cancerous tumours. And not just one type of cancer but many. AOH1996 is just one of a tsunami of new medications and treatments which have the potential to transform the outcome of a cancer diagnosis.
Cancer survival has doubled in the past 40 years, but around 167,000 people still die of the disease in the UK every year. Much of this is down to ever-growing waiting lists – health officials are now considering ways for patients to skip the GP stage and go straight to see specialists.
But, in the meantime, there are also exciting steps forward in medical science.
Kevin Harrington, a professor of biological cancer therapies at The Institute of Cancer Research and an honorary consultant oncologist at the Royal Marsden (RMH) and St George’s Hospital in London, is optimistic that advances in treatment will improve outcomes.
“In 20 years, I confidently expect we will cure a substantially larger number of cancer patients,” he said. “And we will cure them with far smarter and kinder treatments than current approaches.”
This does not mean there will ever be a single cure for cancer, said Dr Claire Bromley, the senior science communications manager for Cancer Research UK.
“Cancer is not a single disease”, she added. “There are over 200 types of cancer, and all of them can be split into different subtypes. It’s unlikely that there will be one silver bullet. However, a combination of many different treatments means we can ultimately beat cancer for everyone.”
Here are the newest breakthroughs to celebrate:
The tumour annihilator
What is it?
The AOH1996 drug is named after Anna Olivia Healy, who was born in 1996 and died aged nine after being diagnosed with neuroblastoma, a rare childhood cancer affecting the nerves.
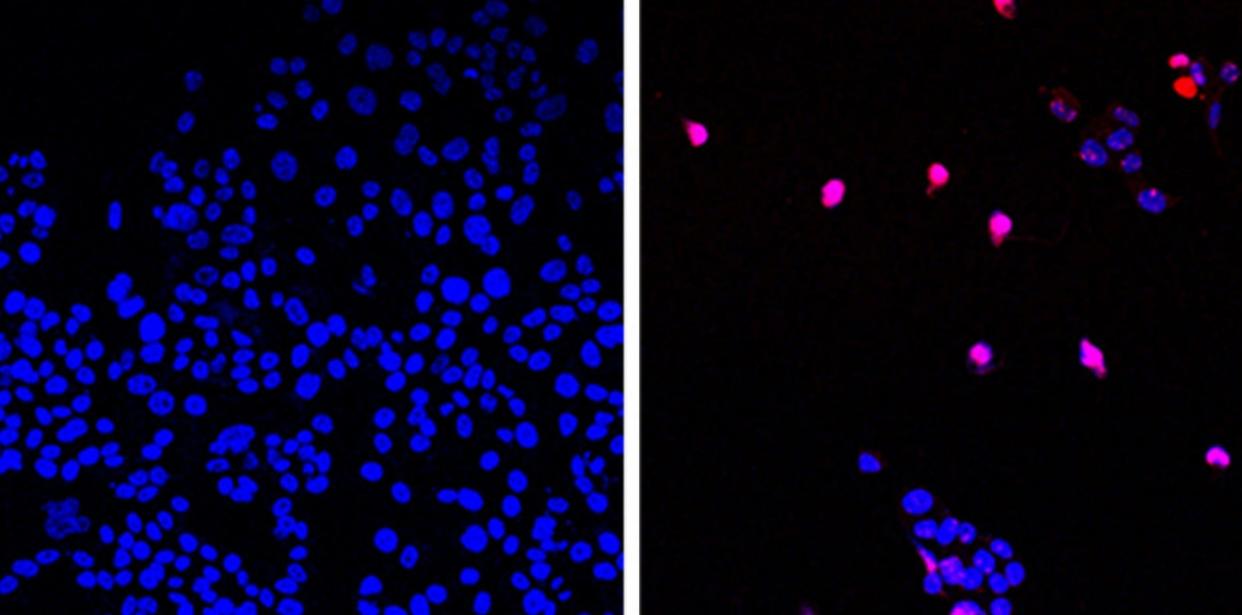
Researchers in the US have developed a molecule that “appears to annihilate all solid tumours” in preclinical research – while leaving healthy cells unharmed.
The experimental cancer-killing pill is taken twice a day and blocks a protein called proliferating cell nuclear antigen (PCNA). In a mutated form, PCNA is critical to the growth and repair of tumours.
“PCNA is uniquely altered in cancer cells, and this allowed us to design a drug that targeted only the form of PCNA in cancer cells, killing tumours while leaving healthy cells untouched,” said Prof Linda Malkas of the department of molecular diagnostics and experimental therapeutics at the City of Hope Hospital, Los Angeles.
What will it treat?
PCNA is found in all cancers, and AOH1996 has shown promise in 70 cell lines, including breast, prostate, brain, ovarian, cervical, skin and lung cancers. It is now being trialled in people for whom standard treatments, such as chemotherapy, have not worked.
When will it be ready?
Prof Harrington said that the drug is “extremely promising”. However, AOH1996 has only just entered phase 1 human trials.
“Even with accelerated trials and evaluation to test AOH1966 for safety and effectiveness, the treatment will take at least five to 10 years to gain approval in the UK,” he said.
A drug to supercharge your immune system
What is it?
Immunotherapy, which harnesses the power of our immune system to attack cancer, has revolutionised cancer treatment.
Nicholas Turner, a consultant medical oncologist at The Royal Marsden NHS Trust and professor of molecular oncology at The Institute of Cancer Research, said: “Twenty years ago, metastatic melanoma [skin cancer that has spread to other organs] had an average survival of around seven months with virtually nobody cured.
“Today, thanks to immunotherapy, survival rates are around 40 per cent.”
But cancers are wily: they can reach out to press “off switches” on our immune cells, calling off their attack. As a result, said Prof Harrington, cures occur in “far too few patients”.
New drugs called “checkpoint inhibitors” block cancer’s ability to hit off switches on the immune system. The best-known checkpoint inhibitors target an off-switch protein called PD-1.
Prof Harrington said: “The problem is that there are dozens of these ‘off switches’. If we find a way to block one, cancer will find another. We need drugs to back cancer into a corner by blocking all the ways it turns off the immune system.”
A new drug, relatlimab, blocks an off-switch protein called LAG-3, making immunotherapy likely to work on more people and more types of cancer.
What will it treat?
Opdualag, a new drug which combines relatlimab with a PD-1 checkpoint inhibitor called nivolumab (Opdivo), has recently been approved by the US Food and Drug Administration for advanced melanoma which cannot be removed by surgery or has spread to other parts of the body.
Other drugs targeting LAG-3 are being trialled for the treatment of multiple myeloma, oesophagal and gastric cancer, among other types of cancers. Opdualag is also being studied in clinical trials of other cancers, including lung, colorectal and liver cancer.
When will it be ready?
The National Institute for Health and Care Excellence is currently evaluating these drugs to treat advanced melanoma with a decision due in December, with more approvals expected in the coming years.
Vaccines that can cure cancer – and prevent it coming back
What are they?
We tend to think of vaccines as treatments we have when we are well. They teach the immune system to recognise a virus so it is destroyed before it can make us sick – or at least make us less sick than we would otherwise be.
However, cancer immunisations are different. While some are being developed to prevent the disease in high-risk patients, most are given when a person has been diagnosed. And they are bespoke treatments, tailored to the patient’s own unique cancer.
Cancer vaccines may be able to cure even advanced, previously terminal cancers and stop cancer coming back and spreading after it has been treated.
Three out of four cancer deaths occur because cancer spreads to other organs, which often happens after a period in which stray cancer cells go to “sleep”, becoming undetectable before waking up and forming tumours.
A cancer vaccine not only trains the immune system to recognise and fight off the initial cancer, but also teaches the immune system to recognise any stray cells so they can be picked off if they become active.
“The key to effective anti-cancer treatments is to create an immunological memory response,” said Prof Harrington. “We want the patient to have a standing army of immune cells trained to recognise and kill cancer if it wakes up.”
There are several different types of cancer vaccines in development which all work in slightly different ways. Many employ the mRNA technology used to create Covid vaccines.
What will they treat?
More than 20 mRNA-based vaccines entered clinical trials by 2021 targeting hard-to-treat cancers including pancreatic and the brain cancer glioblastoma.
When will they be ready?
In July, the Government signed an agreement with the pharma company BioNTech SE to provide up to 10,000 UK patients with precision cancer vaccines by 2030.
Flash radiotherapy
What is it?
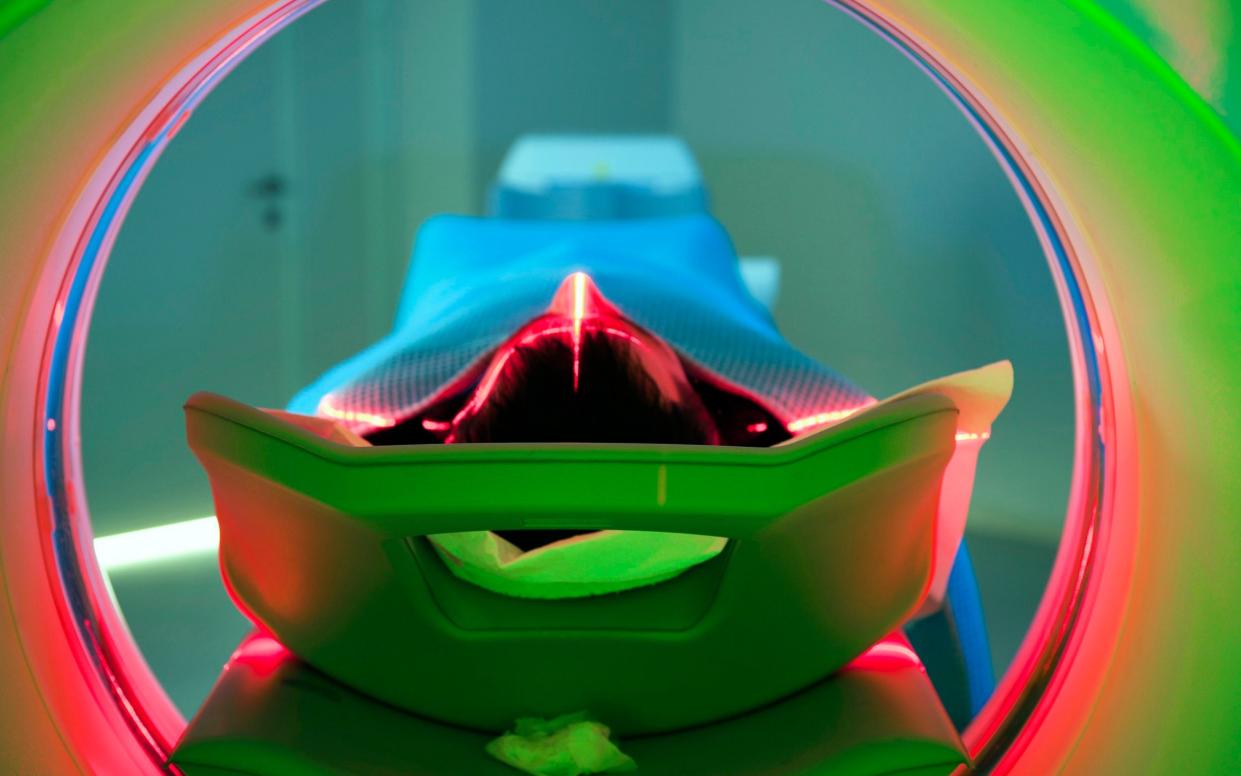
Radiotherapy is often considered an old-fashioned treatment. It uses X-ray energy to kill cancer cells but can also burn and damage healthy tissue in vital organs such as the brain and heart.
However, in flash radiotherapy, radiation is delivered a thousand times faster than in conventional radiotherapy.
A therapeutic dose can be given in a fraction of a second. This intensity damages the DNA in cancer cells but is up to 50 per cent less damaging to normal cells.
Cancer Research UK-funded scientists in the UK have found that flash radiotherapy speeds up oxygen use in the tissues being treated. In normal cells, this creates a condition called hypoxia, and this protects the normal cells from DNA damage.
This protection means clinicians could potentially increase radiation doses to levels that would cause unacceptable side effects with conventional radiotherapy.
What will it treat?
In future, flash could be used for hard-to-kill cancers in the brain, lungs or gastrointestinal area, where healthy tissue surrounding tumours is particularly vulnerable to damage from radiation exposure. “The potential is enormous,” said Dr Bromley.
When will it be ready? So far, flash is only being used in trials. Dr Bromley added: “It could take as long as 10 years before Flash becomes routine.”
Super-viruses that can infect cancers
What is it?
What could be cleverer than giving cancer a disease? That’s the premise of a new breed of engineered viruses created to infect cancer cells but not healthy ones. The viruses essentially trick cancer tumours into destroying themselves.
First, the virus is injected directly into tumours. It then hijacks and replaces the tumour DNA to replicate itself. As the virus grows within cancer cells it bursts them open, and then spreads to other cells while also prompting the immune system to combat the cancer throughout the body.
A new therapeutic virus, RP1, has been created from the herpes simplex virus, which causes cold sores. Tumours are categorised as “hot” or “cold” depending on how much they trigger an immune response. Melanoma is “hot” while breast, pancreatic and prostate cancers are “cold”.
RP1 is designed to work on “hotter” tumours, including in patients for whom immunotherapy hasn’t worked. Sister viruses RP2 and RP3 have been designed to treat more immunologically “cold” tumours.
What will it treat?
In trials, researchers have used an engineered virus to make immunotherapy more effective on brain tumours. It is also being trialled on patients with organ transplants who often develop skin cancers. A quarter of patients saw their cancer disappear.
It has also been trialled in the UK on a small number of last-chance patients with advanced cancers including skin, eye, oesophageal and head and neck cancer. All had failed to respond to other treatments, including immunotherapy.
A quarter saw their cancers shrink and one patient with salivary gland cancer saw his tumour disappear completely. He remains free of cancer 15 months after starting treatment.
When will it be ready?
Availability will depend on the benefit of treatment and the cost of therapy. “In the next three to five years, RP viruses could be available to NHS patients,” said Prof Harrington.
