Chest Tightness: Causes and Finding Relief
A tight chest has many causes, some minor and some serious
Medically reviewed by Brian Bezack, DO
Chest tightness can be a sign of many things, both harmless and severe. While your first thought may be that you are having a heart attack, chest tightness is associated with many other medical conditions, such as:
Musculoskeletal (muscle and bone) injuries
Viral or bacterial infections
Pulmonary (respiratory) diseases
Cardiovascular (heart) diseases
Gastrointestinal (digestive) diseases
Psychogenic (psychological) issues
In the United States, more than seven million people seek emergency care for chest pain each year. But the vast majority of these cases are not caused by a heart or lung condition.
The article describes the different causes of chest tightness, including their symptoms and treatment options. It also explains when chest tightness is a sign of a medical emergency.
Verywell / Laura Porter
Musculoskeletal Causes of Chest Tightness
About half of all people who see a healthcare provider for chest pain are diagnosed with a musculoskeletal) condition. Several can cause chest pain and tightness.
Muscle Strain
Muscle strain can cause chest tightness. If you’ve pulled a muscle—particularly in your chest, abdomen, or upper to middle back—you may experience chest tightness and pain when you're active. In some cases, the strain may be severe enough to cause pain when you breathe.
Strain in the muscles of the chest wall can be caused by:
Overstretching while playing sports or working out
Muscle fatigue
Repetitive or forceful motions
Contact injury, such as from a football tackle
Not warming up muscles before exercise
For chest muscle strains that cause pain and tightness, the first line of treatment usually involves the RICE method:
Rest: Take a break from physical activity. You can restart light activity after a few days but return to resting if tightness and pain return.
Ice: Apply an ice pack to the strained muscle for up to 20 minutes three times a day. This reduces inflammation.
Compression: Wrap a compression bandage around your torso. It can help reduce inflammation and may provide pain relief.
Elevation: Sit upright and maintain good posture. Use extra pillows to prop up your chest at night while you sleep.
You may also want to take over-the-counter (OTC) painkillers like Advil (ibuprofen) and Aleve (naproxen) which are classified as non-steroidal anti-inflammatory drugs (NSAIDs).
See a healthcare provider if you have severe pain, inflammation, or bruising from a chest injury, or if symptoms don't get better within two weeks.
Rib Fracture
Tightness in the chest can be a sign of a broken rib. A rib fracture is a common injury that occurs when one or more bones in your rib cage crack or break. Rib fractures can cause severe chest pain that sometimes makes your chest feel tight.
Rest is important when nursing a rib fracture. Your healthcare provider may also suggest ice application and elevation (and reclining to sleep). Compression is avoided as it has been shown to increase the risk of pneumonia.
Most rib fractures heal on their own in about six weeks. The primary treatment is pain control, such as with NSAIDs or prescription opioid painkillers like Vicodin (hydrocodone/acetaminophen) or OxyContin (oxycodone).
Be sure you don't overdo it while healing. Always get medical care for a fracture and follow your healthcare provider's advice.
Costochondritis
Chest tightness can be a symptom of costochondritis, which is inflammation of the cartilage in the rib cage. It causes chest pain and sometimes chest tightness, often in the middle and upper rib areas. The pain may get worse if you breathe deeply, move, or stretch.
Causes of costochondritis include:
Severe coughing
Chest injury
Infection
Physical strain from repetitious motions or sudden exertion
Treatment generally includes:
NSAIDs
Stretching exercises
For severe pain, opioids or antidepressants for pain control
If your chest hurts more when you lie flat, you may want to prop yourself up on extra pillows or sleep in a recliner.
See your healthcare provider if your costochondritis doesn't improve with home treatment.
Infectious Causes of Chest Tightness
Tightness in the chest can also be caused by infections like the common cold. Chest tightness can also have more serious infectious causes, like shingles. You might also have tightness in your chest from mucus/fluid build-up, inflammation, or other problems.
Acute Bronchitis
Chest tightness when you have a cold or flu can be from inflammation of the large airways of the lungs, known as acute bronchitis. Acute bronchitis is most often caused by a virus.
Excess mucus in your airways caused by bronchitis can restrict breathing and cause:
Coughing
Wheezing
Chest tightness
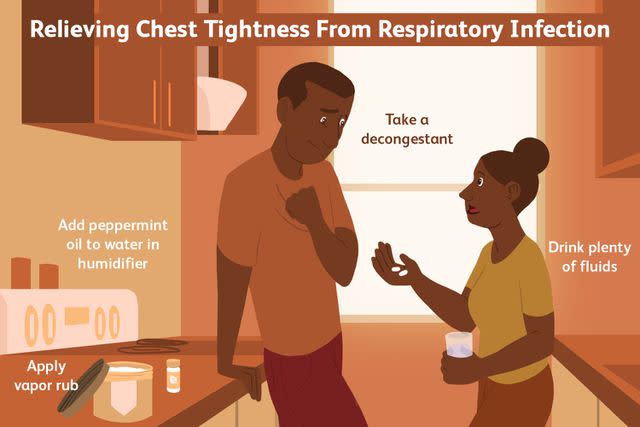
To treat acute bronchitis:
Drink fluids: This thins out mucus. Warm fluids (tea, soup broth, hot water) are especially helpful.
Use a humidifier or take a hot shower: The steam can help clear up congestion. Try using it at night so you can sleep better. Peppermint essential oil in your humidifier helps, too.
Take a decongestant: These OTC drugs help break up mucus and clear congestion. Common ones are Sudafed (pseudoephedrine) and Sudafed PE (phenylephrine). However, while oral decongestants with phenylephrine are safe to take, they are not considered effective decongestants.
Use a vapor rub on your chest/throat: Most rubs have a menthol-based ingredient that may help you feel less congested.
Antibiotics are ineffective against viruses. However, there are antivirals that may help in cases of flu.
When to Seek Medical Care
See a healthcare provider if acute bronchitis is accompanied by:
A fever of 100 degrees or higher
Coughing up bloody mucus
Shortness of breath or difficulty breathing
Symptoms that linger for more than three weeks
Pneumonia
Tightness in the chest can also happen with more serious lung infections. In pneumonia, your lung’s air sacs become inflamed, which can cause them to fill with fluid or pus. Pneumonia can be caused by viral, bacterial, or fungal infections. In the U.S., the most common causes include:
Symptoms of pneumonia include:
Fever and chills
Cough
Mucus that's greenish, yellow, or bloody
Shortness of breath
Chest pain and/or tightness
The chest pain of pneumonia may be sharp and get worse with deep breaths or coughing.
Treatment for pneumonia depends on the cause, severity, your age, and your overall health. If it was caused by a bacteria, you'll likely be given an antibiotic. For viral causes, an antiviral medication may help.
Symptom management consists of:
Fever reducers like NSAIDs or Tylenol (acetaminophen)
Fluids, especially warm ones, to break up mucus
A humidifier or hot shower
Avoiding smoke and other airborne substances that can irritate your lungs
Getting lots of rest
When to Call 911
Call 911 if you have signs of severe pneumonia, including:
Difficulty breathing
Persistent chest pain or pressure
Bluish lips and fingertips
A high fever
Severe cough with mucus
Pneumonia can be life-threatening, especially in children two and under, adults over 65, people with a weak immune system, and people in poor health.
COVID-19
Tightness in the chest can also be a symptom of COVID-19. You might also have other symptoms, such as:
Fever
Runny nose
Congestion
Loss of taste
Shortness of breath
Sometimes, tightness in the chest
Most people with COVID-19 have mild illness and can recover at home. You can treat symptoms with:
Rest
Ample hydration
Tylenol (acetaminophen)
NSAIDs
Antiviral drugs like Paxlovid (nirmatrelvir/ritonavir), Veklury (remdesivir), and Lagevrio (molnupiravir) for people at high risk of severe COVID-19 complications
The sooner you start treatment, the more effective it will be. However, chest tightness may linger in some people with a COVID-19 diagnosis. One study found that COVID chest pain lasts up to two months in 22% of people treated for COVID-19.
When to Call 911
Get emergency treatment for COVID-19 if you have:
Trouble breathing
Persistent chest pain or pressure
Confusion
Difficulty waking up or staying awake
Bluish skin, lips, or nails
Shingles
A feeling of tightness in the chest can also be a symptom of shingles. Shingles is an infection caused by the varicella-zoster virus—the same virus that causes chickenpox. The virus stays in your system forever and in certain circumstances—such as illness, a weakened immune system, or times of high stress—it can reactivate to cause shingles.
Shingles symptoms include:
A painful rash, usually on the torso
Feelings of tightness in the chest (if the pain is severe)
Burning, shooting pains
Tingling, itching, or numbness in affected areas
Fever and chills
Headache
Upset stomach
Your healthcare provider may give you antiviral medications and tell you to take NSAIDs or Tylenol to help with shingles pain. Antibiotic creams for the skin are often prescribed to prevent secondary bacterial infection.
When to Seek Urgent Care
Get urgent medical help if you have shingles blisters on your face, especially near your eyes. This can lead to serious complications, such as blindness, facial paralysis, or encephalitis (brain inflammation).
Lung Conditions That Cause Chest Tightness
Tightness in the chest can be a sign of a problem with the lungs. Asthma and chronic obstructive pulmonary disease (COPD) may immediately come to mind when you think of lung conditions that may cause chest tightness, but there are others—some of which require urgent medical attention.
Asthma
Tightness in the chest is common in people with asthma. If you have asthma, exposure to lung irritants or allergens can cause your airways to constrict and narrow. This leads to:
Chest tightness
Pain
Pressure
Shortness of breath
Wheezing
Cough
Asthma treatments come in two types: immediate rescue treatment for asthma attacks and long-term control medications that prevent attacks. Both types of treatment are usually given via inhalers. Some prescription medications are also available.
A big part of asthma treatment is avoiding the things that set it off. Your healthcare provider can help you identify triggers and work with you on an asthma action plan.
When to Call 911
Call 911 or go to the nearest emergency room if an asthma attack is severe, causing:
Rapid breathing (30 or more breaths per minute)
Blueish lips or nails
Flaring nostrils when you inhale
Retraction of the skin between the rib as you inhale
A feeling that you cannot get enough air
Related: What Is Chest Congestion in Asthma?
Chronic Obstructive Pulmonary Disease (COPD)
Chest tightness can happen if you have COPD. Shortness of breath from constricted airways is the main symptom, but you may feel chest tightness or like something is wrapped around your chest—even while at rest. You could also have a cough and a lot of mucus.
COPD is the result of irritation and damage to your lungs and airways, which is often caused by long-term exposure to cigarette smoke, air pollution, or chemical fumes.
COPD is often treated with:
Inhalers
Nebulizers (machines that deliver medication as a mist)
Corticosteroids such as prednisone, hydrocortisone, and methylprednisolone
Phosphodiesterase-4 inhibitors such as Otezla (apremilast), Eucrisa (crisaborole), and Daliresp (roflumilast)
When to Call 911
Seek emergency care if you experience a severe COPD exacerbation (flare-up) with symptoms such as:
Chest pain
Breathing or talking difficulty
Fever
Racing heartbeat
Blue lips or nails
Slurred speech
Confusion or disorientation
Dizziness
Difficulty waking up
Related: Why COPD Causes Chest Tightness
Pulmonary Hypertension
Tightness in the chest can be a sign of a chronic lung disorder. Pulmonary hypertension (PH) is a progressive lung disease in which the arteries that carry blood from the heart to the lungs become narrow. It can be caused by many things, including:
Autoimmune diseases that damage your lungs
Birth defects
Blood clots in the lung (pulmonary embolism)
Symptoms of PH include:
Shortness of breath from everyday activities, like walking up the stairs
Fatigue
Dizziness
Chest pain
Chest tightness when strain is placed on the heart during activity
Swelling (edema) in the legs and ankles
Weakness
Blue lips or skin
Pulmonary hypertension can't be cured, but medications can help manage it. They include:
Calcium channel blockers to decrease blood pressure
Diuretics to rid the body of excess fluid that puts pressure on the heart
Oxygen therapy, in some cases
Pleuritis
Tightness in your chest can be a sign of inflammation. Pleuritis (also called pleurisy) is inflammation of the pleura—the large, thin layer of tissue that separates your lungs from your chest wall. It's caused by various things, including:
Viral or bacterial infection
Some cancers, such as lung cancer, lymphoma, and mesothelioma
Blood clot in the lung
Symptoms of pleuritis include:
Sudden and sharp pain in the chest when breathing
Pain with coughing or deep breaths
Ongoing chest pain and tightness
Shortness of breath
Fever
Body aches
Pleuritis generally resolves when the cause is successfully treated, such as by clearing up an infection with antibiotics or antivirals. To manage pain from pleuritis, your healthcare provider may suggest NSAIDs or, for severe pain, steroid drugs to reduce inflammation.
You should make an appointment with a healthcare provider if you have symptoms that could be from pleuritis, especially if you have a condition that could cause it.
When to Call 911
Call 911 or seek emergency care if you have symptoms of severe pleurisy, including:
Severe chest pain
Coughing up blood
Nausea
Related: Alcohol, Antibiotics, and Healing: What Happens?
Pneumothorax
Tightness in the chest can have serious, even life-threatening, causes. Pneumothorax (collapsed lung) occurs when a hole in the lung allows air to escape and fill the space between the lung and chest wall. The trapped air puts pressure on the lung, so it cannot expand as it should when you take a breath. This can cause:
Chest tightness
Sudden, sharp chest pain that's worse when you cough or breathe deeply
Shortness of breath
Being easily fatigued
Rapid heart rate
Bluish skin (due to lack of oxygen)
Pneumothorax can be caused by chest trauma, extreme pressure on the lungs, or lung diseases including:
A minor collapsed lung can resolve on its own in a few weeks. In larger collapses, the air needs to be removed. A healthcare provider can place a chest tube between your ribs to drain the air and let the lung expand properly.
Other treatments include oxygen therapy and surgery to prevent a future collapse.
Pulmonary Embolism
You may feel tightness in your chest if you have a blood clot. Pulmonary embolism is a sudden blockage of an artery in the lungs, most often caused by a blood clot that forms somewhere else and travels to the artery. It can cause low oxygen levels in your blood, which may damage your lungs and other organs.
Not everyone has symptoms of pulmonary embolism. Those who do may experience:
Sudden shortness of breath
Chest pain and tightness that's usually worse with breathing
Anxiety
Dizziness or fainting
Irregular heartbeat or racing heart
Coughing up blood
Sweating
Risk factors for pulmonary embolism include:
Genetic conditions that raise the risk of blood clots
Family history of clotting disorders
Injury (especially to the legs)
Surgery, especially orthopedic procedures
Limited mobility (from things like prolonged bed rest or long-distance air travel)
Previous clots
Getting older
Cancer and some cancer treatments
Some medical conditions (like heart failure, COPD, high blood pressure, or stroke)
Smoking cigarettes
This condition requires immediate medical attention.
Treatments include:
Blood-thinning medications such as warfarin
Intravenous (IV) "clot buster" medications (called thrombolytics or fibrinolytics)
A filter in the vena cava (a large blood vessel carrying blood to the heart) to keep clots out
Surgery to remove the clot (pulmonary embolectomy)
Percutaneous thrombectomy (a hollow tube in the blood vessel is used to remove or dissolve the clot)
When to Call 911
A pulmonary embolism is a potentially life-threatening medical emergency. Call 911 or go to the emergency room if you have symptoms, especially if accompanied by signs of deep vein thrombosis (DVT). It is not uncommon for both to occur together.
Symptoms of DVT include:
Swelling of one leg only
Throbbing or cramping pain in the calf or thigh
Warm skin around the painful site
Dark red skin around the painful site
Hard, sore, or swollen veins in the affected leg
Heart Conditions That Cause Chest Tightness
Tightness in your chest might make you think you have a heart problem, and it's true that it can be a sign of something wrong in your cardiovascular system.
Chest pain and tightness may be caused by a number of heart-related conditions, some of which are serious. It's important to see your healthcare provider, who can help to determine if you have any of the following concerns.
Coronary Artery Disease
A tightness in your chest can be a sign of coronary artery disease (CAD). CAD is caused by a build-up of cholesterol and other substances in the coronary arteries (large blood vessels of the heart). That makes the arteries narrow or can block them entirely. This can cause a heart attack, which is often the first sign of CAD.
Narrowed arteries can cause:
Angina (chest pain, tightness, heaviness, pressure, fullness, or squeezing)
Pain or discomfort in the arms or shoulders
Weakness
Light-headedness
Nausea
Cold sweat
Shortness of breath
Risk factors for CAD include a family history of heart disease (especially before age 50), excess body weight, an unhealthy high-fat diet, and smoking.
If you have CAD, your healthcare provider may prescribe drugs that:
Help to improve blood flow
Widen arteries
Prevent blood clots
Lower your cholesterol
Lower your blood pressure
Ease chest pain
Surgery may be an option for more serious cases of coronary artery disease. They include:
Percutaneous coronary intervention (PCI): Opens narrowed or blocked arteries, usually by using a stent to prevent future narrowing
Coronary artery bypass grafting (CABG or "heart bypass"): Re-routes blood through other blood vessels to bypass the blockage; usually done in severe CAD involving multiple arteries
Transmyocardial laser revascularization or coronary endarterectomy: For angina from CAD; reserved for when other treatments don't work or the risk of those treatments is too high
Learn More: How Coronary Artery Disease Is Treated
Mitral Valve Prolapse
Tightness in the chest can occur if there's a problem with the heart valves. In mitral valve prolapse (MVP), the valves between the left atrium and left ventricle of your heart develop a bulge (prolapse). That means they can't close correctly and blood can flow backward through the valves.
MVP can cause a heart murmur (a "swooshing" sound when listening to the heartbeat) and a number of other symptoms, including:
Chest tightness or pain, which can be recurrent and incapacitating, and may occur even at rest
Fast and/or irregular heartbeat
Blood clots, heart attack, or stroke (in severe cases)
MVP's cause is unknown, but it may have a genetic component. Other conditions may contribute to its development, including:
Inherited connective tissue diseases such as Marfan's syndrome
Coronary artery disease
Heart attack (myocardial infarction)
Rheumatic heart disease
Hypertrophic cardiomyopathy (an enlarged left ventricle)
MVP isn't usually serious and may not require treatment. If it does, treatment may include:
Beta-blocker drugs like Tenormin (atenolol) or Lopressor/Toprol XL (metoprolol)
Blood thinners like Jantoven (warfarin) or aspirin
Surgery like mitral valve repair or replacement
Even if you don't need treatment, your healthcare provider should monitor the condition.
Related: What Is Paroxysmal Atrial Fibrillation?
Pericarditis
Feeling tightness in your chest can be a sign of inflammation. Pericarditis is inflammation of the protective membrane surrounding the heart (pericardium). This thin tissue allows the heart to change in size with each heartbeat.
When inflamed, the membrane can rub against the heart and cause:
Sharp and stabbing chest pain
Pain radiating to the neck, shoulder, back, or abdomen
Worsening pain when lying down or taking deep breaths
Swelling of the feet, ankles, and legs
Anxiety
Dry cough
Fatigue
Pericarditis is most common in men between the ages of 20 and 50. The cause is often unknown, but it may be linked to:
Viral infections that cause a chest cold or pneumonia
Bacterial infections (less common) or fungal infections (rare)
Cancer
Autoimmune disease
HIV/AIDS
Hypothyroidism (underactive thyroid)
Rheumatic fever
Tuberculosis
Heart attack or trauma to the heart or chest
Radiation therapy to the chest area
Some cancer drugs or immunosuppressants
Mild pericarditis may clear up on its own. More serious cases require treatment, especially if it becomes potentially life-threatening. Treatments for pericarditis include:
NSAIDs
Corticosteroids to lower inflammation
Antibiotics for bacterial infections
Antifungals for fungal infections
Diuretics to remove excess fluid, which may contribute to inflammation
For cases with severe fluid buildup, healthcare providers may perform a procedure to drain the excess fluid.
Hypertrophic Cardiomyopathy
Tightness in your chest could be a sign that you have a heart condition. For example, hypertrophic cardiomyopathy (HCM) involves abnormally thick walls of the left ventricle, one of the heart's four chambers. The thickness makes it harder for the heart to pump blood. This is believed to be due to abnormal genes affecting the heart muscle.
HCM can be obstructive (blocking or reducing the flow of blood) or nonobstructive. Most people have the obstructive type.
Symptoms of HCM often get worse with exertion. They may include:
Chest pain and tightness
Shortness of breath
Abnormal and/or rapid heartbeat
Dizziness, lightheadedness, and fainting
Swelling in the feet, ankles, legs, and abdomen
Fatigue
HCM is generally treated with medications and medical procedures. Treatments may include:
Medicines that correct the abnormal heart rhythm
Blood thinners to reduce blood-clot risk
A pacemaker to control the heart rhythm
An implanted defibrillator that corrects life-threatening heart rhythms
A heart-healthy lifestyle is recommended for managing HCM as well.
Coronary Artery Tear
Tightness in your chest can be a medical emergency that requires immediate medical attention. For example, chest tightness can be a sign of a rare condition called spontaneous coronary artery dissection (SCAD), which happens when there is a sudden tearing of a blood vessel in the heart.
When the artery wall tears, blood can get trapped between the layers of the wall and cause a bulge that restricts or blocks the flow of blood. That can cause a heart attack.
The causes of SCAD are unknown. It happens most often in biological females who:
Are otherwise healthy
Have few or no heart-disease risk factors
Recently gave birth (30% of cases)
Are having a menstrual period
When SCAD happens in biological males, it's usually after extreme exertion, such as a chest that feels tight when you run. About 80% of SCAD cases are in people who are young, healthy, and active. For that reason, it's important for everyone to know the signs of a heart attack:
When to Call 911
Call 911 or get to an emergency room right away if you have signs of a heart attack, including:
Chest pain or tightness, usually in the center or left side of the chest
Chest pain that lasts for more than a few minutes, or goes away and comes back
Pain that radiates to the jaw, neck, back, arm, or shoulder
Weakness, lightheadedness, or fainting
Shortness of breath
If you have SCAD once, you're at high risk of having it again. It’s important to adopt a heart-healthy lifestyle and see a cardiovascular specialist for regular monitoring.
Gastrointestinal Causes of Chest Tightness
Some gastrointestinal issues can cause tightness in the chest and pain in the chest area. The pain is felt near the heart but actually comes from digestive organs in that area, including the stomach and esophagus.
Gastroesophageal Reflux Disease (GERD)
A tight feeling in your chest could be a sign of acid reflux. Gastroesophageal reflux disease (GERD) involves chronic acid reflux, which is when stomach acid pushes back up into your esophagus (the tube that runs from your throat to your stomach).
Acid reflux is caused by problems with a structure called the lower esophageal sphincter (LES). The LES opens when you swallow, then is supposed to shut tightly so stomach contents stay out of the esophagus. When it's weak or doesn't close properly, reflux occurs.
GERD symptoms include:
Regurgitation (stomach contents rising up into the throat or mouth)
Chest tightness that may feel like a weight on your chest or a crushing pain
Nausea
Problems swallowing
Chronic cough
Hoarseness
GERD is treated with over-the-counter (OTC) or prescription medications such as:
Antacids like Tums or Rolaids
Proton pump inhibitors like Prilosec (omeprazole), Nexium (esomeprazole), or Protonix (pantoprazole)
H2 blockers like Tagamet (cimetidine) and Zantac (famotidine)
Lifestyle changes are also recommended for GERD, including:
Reaching and maintaining a healthy weight
Not smoking
Changing your diet and eating habits
Elevating your head while you sleep
Some surgeries may help, but due to a greater risk of complications than medications, they're usually reserved for when symptoms don't improve with medications and lifestyle changes.
Related: The 7 Best Antacids
Hiatal Hernia
Tightness in the chest can be caused by a hiatal hernia. This condition happens when the top part of your stomach bulges through an opening in the diaphragm muscle that separates your chest and abdomen. That causes upward pressure that can lead to chest tightness, acid reflux, and GERD.
Not every hiatal hernia causes symptoms. When they do, symptoms may include:
Heartburn
Problems swallowing
Dry cough
Bad breath
Nausea and/or vomiting
Breathing problems
Erosion of your tooth enamel
Hiatal hernias can be caused by injury, birth defects, or weakness of muscles surrounding the area. Your risk of one increases as you age, if you smoke, or if you have obesity.
If you don't have symptoms, your hiatal hernia doesn't need to be treated. For symptomatic cases, treatments include:
Eating small meals
Avoiding foods that trigger symptoms
Not smoking
Avoiding alcohol
Weight loss, if you have obesity
Antacids
GERD medications
If all else fails, surgery to fix the hernia may be an option.
Peptic Ulcer Disease
Tightness in your chest can mean you have peptic ulcer disease, which causes painful ulcers (sores) in the lining of the stomach or duodenum (the first part of the small intestine). They're caused by stomach acids damaging the lining of these organs.
Those acids are naturally present and don't usually cause damage. Something has to change in order for the acid to become a problem. The mechanism is different depending on the cause:
Long-term use of NSAIDs: These drugs reduce your body's production of an enzyme that protects the stomach lining from acid.
Heliobacter pylori (H.pylori) infection: These bacteria irritate the stomach and duodenum and also damage their protective mucus coating.
Zollinger-Ellison syndrome: This rare condition causes tumors in the pancreas and duodenum that release large amounts of the hormone gastrin, which triggers the production of excess stomach acid.
The primary symptom of peptic ulcer disease is burning pain in the stomach, which can sometimes feel like chest tightness and pain.
Other symptoms may include:
Bloating
Burping
Nausea
Poor appetite
Vomiting
Unintended weight loss
Treatment of peptic ulcers varies by the cause and may include:
Antacids
Proton pump inhibitors
Stopping NSAIDs
Antibiotics for H. pylori infection
Procedures to stop bleeding from ulcers
Gallstones
A tight feeling in your chest could be a sign of gallstones, which are like pebbles that form in your gallbladder. The gallbladder releases bile to help with digestion, but gallstones can block the ducts it travels through. That makes bile build up and causes a gallbladder attack.
Gallbladder attacks can include pain in your upper right abdomen after eating, which may feel like chest tightness in some cases. The pain can be severe and may last for several hours. Attacks are more common after heavy meals, which makes them most likely in the hours after you eat dinner.
If your gallstones don't cause symptoms, they may not need treatment. However, if you've had one gallbladder attack, you're likely to have more, so let your healthcare provider know about it.
The most common treatment for gallstones is removing the gallbladder. This surgery is called a cholecystectomy. If your health makes surgery too risky for you, your provider may suggest:
A procedure called endoscopic retrograde cholangiopancreatography to remove a gallstone that's stuck in a bile duct
Medications including Actigall (ursodiol) or Chenix (chenodiol) that break up gallstones; this may take months or years
A procedure called shock-wave lithotripsy to break up stones into small pieces, sometimes used along with medications
When to Seek Medical Care
Seek immediate medical care for a gallbladder attack that causes:
Upper abdominal pain lasting for several hours
Nausea and vomiting
Fever or chills
Jaundice (yellowing of the skin or eyes)
Cola-colored urine
Pale stools
Esophageal Disorders
A tightness in your chest might actually be related to a problem in your throat. Some esophageal disorders can cause chest tightness and pain, including:
Esophageal contraction disorder (muscle problems that affect swallowing)
Esophageal hypersensitivity (sensations that are similar to GERD)
Esophageal rupture (a tear in the esophagus)
The causes of these conditions aren't yet fully understood, but they appear to be more common in people who:
Are young
Drink a lot of alcohol
Smoke frequently
Have a lot of anxiety
Have functional GI disorders such as irritable bowel syndrome (IBS) or functional bloating
Esophageal disorders may be treated with:
Proton pump inhibitors
Antidepressant medications
Theophylline (a drug that relaxes the throat)
Cognitive behavioral therapy (for some people)
As a last resort, surgery may be recommended for some conditions.
Anxiety Attacks
Tightness in the chest can also be related to your mental health. When you feel anxious, it can trigger a stress response in the body known as fight-or-flight mode. Symptoms of an anxiety attack include:
Rapid heart rate
Chest tightness
Abdominal cramping
Diarrhea
Muscle pain
Rapid, irregular heartbeat
Rapid breathing
Treatments for chest tightness due to anxiety include:
Breathing exercises: Taking slow, deep breaths can help you to relax.
Grounding techniques: Bring your attention to the present moment. Focus on how your body feels and try to slow your thoughts and breathing.
Exercise: Try walking, running, or hitting a punching bag.
Your healthcare provider may also suggest anti-anxiety medications, mental health counseling, or relaxing activities such as yoga or tai chi.
Summary
Chest tightness can be caused by conditions in different parts of the body, not just your heart and lungs. Many of these causes are related to lung or heart conditions or injury, but an infection, musculoskeletal problems, or digestive disorders can also cause tightness in the chest. Even anxiety or emotional upset can cause chest tightness.
Read the original article on Verywell Health.

