Kids Are Losing Health Insurance And GOP Policies Look Like A Big Reason Why
The number of children getting health coverage through two large government programs fell by more than 800,000 last year, according to a new report from Georgetown University.
The enrollment decline could be an indicator that the number of kids without any kind of health insurance went up in 2018, one year after that figure rose for the first time in a decade. It’s impossible to be sure, because firm, up-to-date estimates on the number of uninsured children won’t be available until the release of new census data in the fall.
The Georgetown paper also doesn’t say definitively why fewer children are enrolled in the government programs. But it gives a list of the most likely causes, including reductions in outreach funding and new paperwork requirements for families trying to demonstrate their eligibility. Pretty much of all of the probable factors are the handiwork of Republicans ― some in Washington, some in state capitals.
Most of those changes haven’t received a lot of publicity. But their impact on the well-being of children could be serious and long-lasting.
“If children losing Medicaid and CHIP are becoming uninsured, there are many negative consequences for them and their families, including less access to primary and preventive care, increased exposure to medical debt, and longer term educational and economic impacts,” the researchers wrote.
It’s Probably Not The Economy
The new report focuses on Medicaid and the Children’s Health Insurance Program, both of which states administer under federal guidelines and with varying levels of federal financial support. Each state operates its programs a little differently, but together they provide coverage to 4 out of every 10 Americans less than 18 years old.
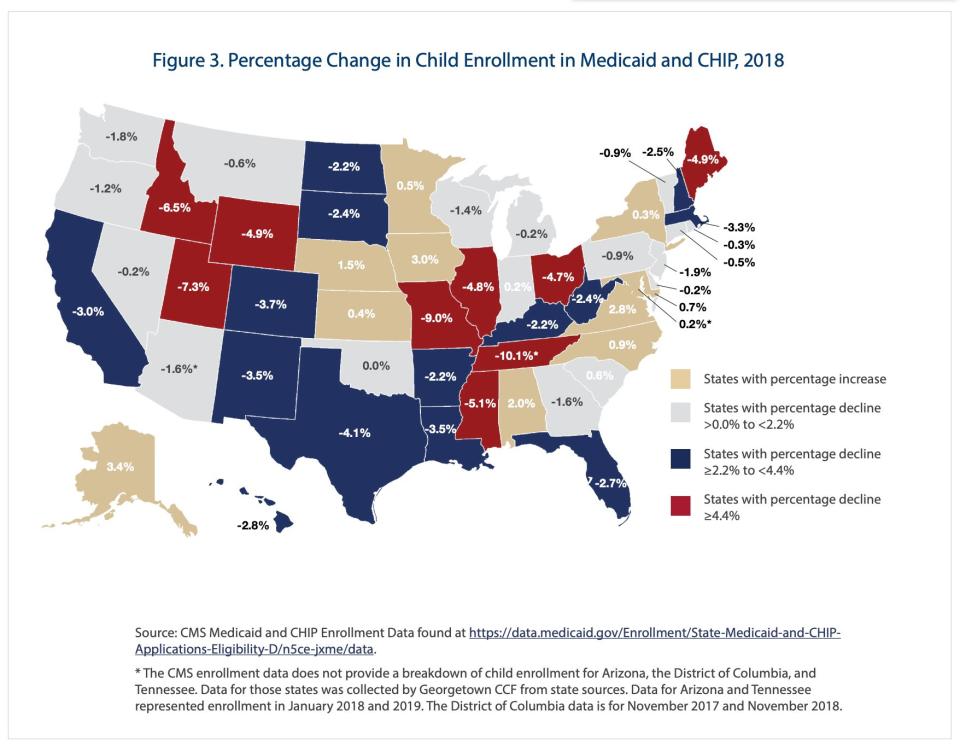
Enrollment in Medicaid and CHIP fell in 38 states between the end of 2017 and the end of 2018, the report says, citing official federal data. Enrollment rose in 12 states plus the District of Columbia.
In theory, the enrollment decline could be a sign that, with both employment and incomes rising, fewer families with children need insurance from the government. But Georgetown researchers Tricia Brooks, Edwin Park and Lauren Roygardner found scant evidence that the economy explained the trend.
They noted, among other things, that preliminary census data has shown no increase in children with employer-sponsored coverage. (The census data actually revealed a decline, though it was not statistically significant.)
“While employment gains continued to be steady in 2018, there was no clear surge in the trend for parents that would explain why nearly 1 million children were disenrolled from Medicaid due to increased income,” the researchers wrote in the report.
It’s Likely These National And State Changes
Having concluded that the economy could not explain most or even much of the enrollment decline, the researchers pointed to a series of national and state-specific factors that more likely played a significant role.
Among the national factors was the end of the Affordable Care Act’s individual mandate penalty, which the 2017 GOP tax law reduced to zero. The penalty, while in force, encouraged people to get insurance or at least to look for it. Many of them discovered, to their surprise, that they were eligible for free or nearly free coverage through a government program.
Another likely reason Medicaid and CHIP enrollment fell, according to the report, was a series of unilateral actions by the Trump administration. Those moves included more aggressive deportations as well as proposals that would make it harder for immigrants who had previously received Medicaid to extend visas or get permanent legal status. Previous studies, the report notes, have shown that both of those factors discourage even legal residents eligible for coverage from signing up.

And then there were a series of drastic cuts in spending on advertising for HealthCare.gov and the counselors who help people to enroll in government insurance programs. Publicly, administration officials said that they were trying to spend taxpayer dollars more responsibly and that the outreach efforts didn’t work. But they had studies showing just the opposite.
On top of these nationwide changes, several states are in the process of making it more difficult for people either to sign up for or to stay on government insurance.
This is not a new phenomenon, the report explains. Officials eager to limit or reduce enrollment in public programs have long known that adding paperwork requirements is an efficient, politically easy way to do it. But the effects are particularly visible now, the report says.
Tennessee Offers A Case Study
In Tennessee, enrollment in Medicaid and CHIP fell by more than 10 percent last year. That was the largest drop in any state and the main reason, almost certainly, was more aggressive scrutiny of renewals that started in late 2016. Tennessee families on Medicaid or CHIP now get a printed renewal packet that is 98 pages long and requires 17 full pages of personal and financial information, much of which the state already has.
The decline first came to light through investigative reporting by Nashville Tennessean reporter Brett Kelman. State officials have said lower enrollment is simply a byproduct of the state overseeing the programs more carefully and fewer people needing government help with health care. But Kelman found widespread evidence that eligible people were falling off the rolls, in many cases because notifications of impending disenrollment never reached them.
Michelle Johnson, executive director of the Tennessee Justice Center, told HuffPost that her organization is getting calls from parents “all over the state,” sometimes after they show up at the hospital only to discover their coverage has lapsed. Officials at the center, which advocates for low-income residents, had warned the new process could have this effect. Now, Johnson said, people trying to get back on the programs are finding it takes weeks or months.
Tennessee officials insist their goal is simply to run efficient programs and make sure people who need care get it. But Johnson said the new enrollment procedures ― and lack of alarm over their dramatic effects ― are likely byproducts of the antipathy those officials feel toward all government-sponsored health insurance.
She noted that Tennessee is among the 14 states that refuse to use the Affordable Care Act’s funds to expand Medicaid to more low-income people and that, right now, it is seeking permission to switch the way it receives federal Medicaid funding to a “block grant,” which would likely mean reductions in whom or what it covers.
Tennessee officials “have been very hostile to any sort of government programs related to health care,” Johnson said. “Spending taxpayer money the way it’s supposed to be spent ― on health care for people who need it ― has gone very out of vogue here.”
Love HuffPost? Become a founding member of HuffPost Plus today.
This article originally appeared on HuffPost.

