How This Mother Went to Extremes to Help Her Mentally Ill Son: 'He Knows He's Locked up Because of Mom'

Courtesy Frances Musgrove Frances Musgrove with her son Justin in December.
Frances Musgrove recalls the day a psychiatrist told her that her son Justin, then 22, would probably never work again.
Justin had battled mental illness for years. He'd been arrested, hospitalized, lived on the streets and become increasingly psychotic, and — as an adult — was free to refuse care and treatment. But to never work again?
That hit Musgrove hard.
"I can still remember it physically," she says. "I'd just been told, basically, that Justin was doomed. I wanted to drive our car off a cliff with us both inside but I didn't want us left mangled because that would be worse, so I couldn't do it."
Justin, 41, is one of 14 million-plus Americans who suffer from serious mental illness, including schizophrenia and bipolar disorder, which usually emerges in late teens or early adulthood. Some mental-health experts believe that psychotic breaks are the climax of a long buildup, rooted in neurobiological changes in the brain that can begin as much as a decade earlier.
At least half of those living with schizophrenia experience a neurological symptom called anosognosia, which impairs people's ability to perceive their illness. This feature presents many obstacles, says Xavier Amador, a clinical psychologist who's CEO of the nonprofit Henry Amador Center on Anosognosia on Long Island, N.Y. "It's not surprising that these patients refuse support," he says, "so the person is in the psychiatric emergency room, they're hearing voices, they're delusional about the CIA, and the last thing they want is any treatment."
And when someone's refusing treatment, they often end up breaking the law, says Amador. "They may stalk somebody, they may stay in the middle of the street, talk to their voices, so they end up in the criminal justice system."
Justin was well into anosognosia and had realized most of those behaviors by his mid twenties. Although he'd been diagnosed with bipolar disorder at age 15 (the confirmation of schizoaffective disorder wouldn't come until his early 30s), he was scattered in his medication compliance and, says his mother, "not understanding that he's doing anything wrong at all. Nothing is his fault. He doesn't know he's having delusions or that he's paranoid. I can't tell you how many times he accused me of having Munchausen's [syndrome by proxy] because I tried to make him take his medication."
While incarcerated, Justin told his mother that the people there were performers brought together just for him.
"I would bawl my head off all the way home from visiting him in jail," says Musgrove, a retired florist who lives in Phoenix. "Then I would be able to calm down by saying the rosary just as quick as possible. I felt really alone."
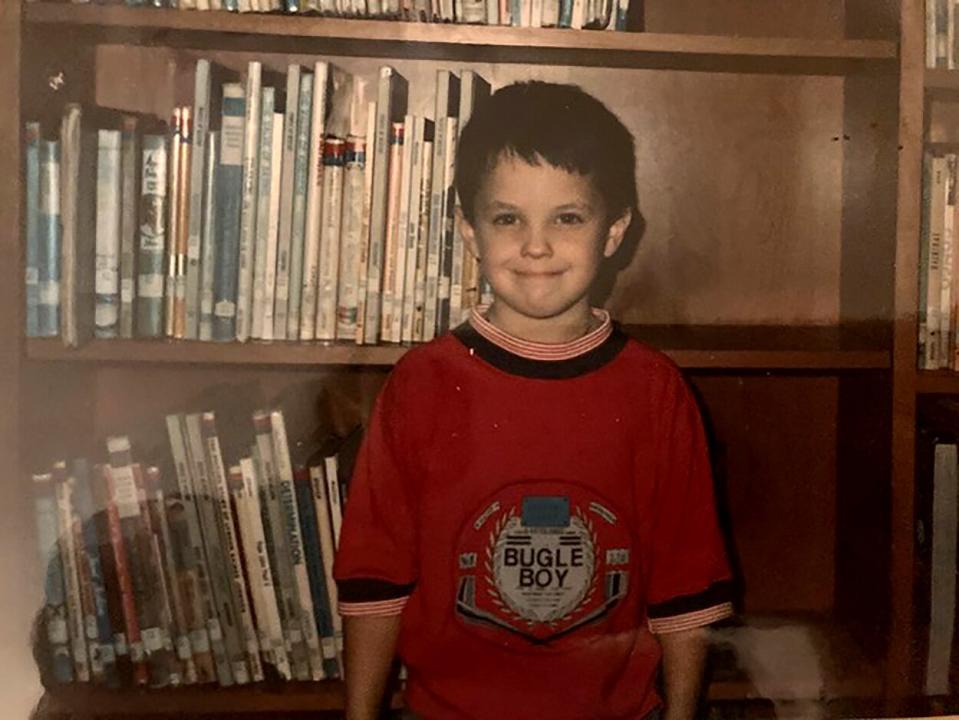
courtesy Frances Musgrove Justin at the age of 7.
Isolation and hopelessness are common among family members who have loved ones suffering from serious brain diseases, says Linda Mimms of San Diego, vice chair of the Schizophrenia & Psychosis Action Alliance. "How would you feel if the doors were slammed in your face when you're just trying to obtain medical care for your loved one, care that would give them their lives back?"
Anosognosia takes away a person's decision-making capacity to direct their own care, and some civil-rights groups advocate for people's power to make their own medical choices. "But in psychosis, they're unable to do this," says Mimms. "Leaving people untreated condemns them to homelessness, incarceration, and terrible deaths. What if this was our answer to Alzheimer's and Parkinson's patients, who experience similar symptoms?"
RELATED: Author Grace Cho Shares Her Mother's Story of Developing Schizophrenia at 45: 'I Was Terrified'
But there are some bright spots. Amador has developed a science-based approach called LEAP (Listen, Empathize, Agree, Partner), a relationship-building style of communicating that encourages someone with anosognosia to accept treatment. Trying to convince someone with anosognosia that they are sick is pointless, he says. "All you're going to do is alienate them," Amador says. "Stop educating and start listening and engaging with the person and following their lead to find out what they want, what they think the problem is. You work with them to marry their definition of the problem with yours."
He also points to fresh investments in the health care industry such as new medications and therapies (cognitive behavioral therapy for psychosis, for example, in which the intensity of hallucinations and the severity of delusions can be reduced through talk therapy) that provide hope for patients.
After some years on the streets and at least 80 hospitalizations, Musgrove has managed to help Justin achieve some relief. He is living in a dual-diagnosis (mental health and drug use) facility where he is cared for and medically treated.
"Justin still has no insight into his mental illness," says Musgrove. "He just knows he is locked up because Mom makes that happen. The situation isn't ideal but it's a far cry from a year ago when he was on the streets and had been hit by a car, severely injured and left to fend for himself. I'm thankful he is safe."

