Budget cuts, dating apps, and unsafe sex — why STDs in America are at an all-time high
Rates of sexually transmitted diseases (STDs) in the United States are at an all-time high, according to new preliminary data released by the Centers for Disease Control and Prevention (CDC).
Nearly 2.3 million cases of chlamydia, gonorrhea, and syphilis were diagnosed in the U.S. in 2017, the CDC data reveals. This blew away numbers from 2016 by more than 200,000 cases, making this the fourth consecutive year that STD cases have sharply increased in the country.
The CDC analyzed data from 2013 and 2017 and found the following:
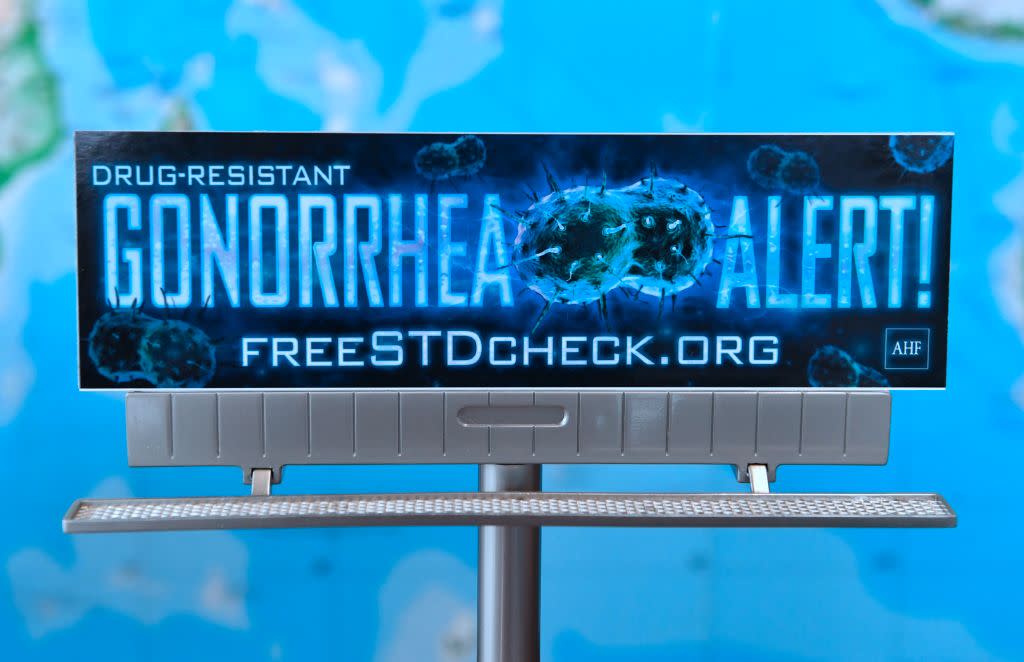
Gonorrhea cases increased 67 percent during that time period and nearly doubled among men.
Diagnoses of primary and secondary syphilis (the most infectious stages of the disease) increased 76 percent, with gay, bisexual, and other men who have sex with men making up almost 70 percent of cases.
Chlamydia remains the most common STD reported to the CDC, with more than 1.7 million cases diagnosed in 2017. Nearly 45 percent of those cases were among 15- to 24-year-old women.
All of these STDs are treatable with antibiotics, the CDC points out, but most go undiagnosed and untreated, which can cause health problems such as infertility, ectopic pregnancy, stillbirth, and an increased HIV risk. But while the CDC shared the data, it didn’t reveal why STDs seem to be increasing so much, and at such a fast rate.
So what is the cause?
“I don’t think that there is just one reason why there is an increase in [sexually transmitted infections] in the USA but rather the perfect storm of several reasons,” Michael Cackovic, MD, an ob-gyn at the Ohio State University Wexner Medical Center, tells Yahoo Lifestyle. “There have been severe cuts to public health systems and clinics that provide care for many people with STIs. … [And] anonymous sex is again on the rise due to the availability of dating apps like Tinder and Grindr.”
Many women also no longer see their ob-gyn for annual wellness checks like they used to thanks to changes in cervical cancer screening recommendations that now say women can opt to have a Pap test every three years, G. Thomas Ruiz, MD, lead ob-gyn at Orange Coast Medical Center in Fountain Valley, Calif., tells Yahoo Lifestyle. “For many women, if they’re not coming in for their Pap smears, they’re not coming in for their wellness exams,” Ruiz says. Women are usually tested for STDs during those wellness exams, and if they’re spacing them out and they have an STD, they’re more likely to unknowingly pass it on to others during that time, he says. “By the time they’re actually diagnosed, they may have already spread it to a lot of people,” Ruiz says.
Another problem is a lack of condom use. “I don’t think a lot of people are using barrier methods,” Ruiz says. “It’s important for doctors to remind people that, hey, condoms are good for things other than birth control.” It’s also important for patients to understand that they should use a barrier method even if they’re on another form of birth control, Ruiz says. “The pill will protect you from getting pregnant, but it will not protect you from STDS,” he says.
“People have also gotten complacent with STIs,” says infectious disease expert Amesh A. Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security. “Most people believe that they’re easily treatable and not that big of a deal, but that’s not the case when you see that gonorrhea is becoming harder to treat.”
Both doctors and patients may avoid talking about STDs as well, which compounds the problem, Adalja says. “Many physicians don’t talk about this with their patients, and many patients don’t volunteer symptoms,” he says.
Ultimately, this needs to be addressed by public health officials and doctors alike, Adalja says. The way in which it’s discussed matters too, Cackovic says. “We need more federal and state funding for public health and more programs teaching safe sex as opposed to just abstinence,” Cackovic says. “Abstinence is fine for some groups, but others will still have sex but may be less likely to seek medical care due to the stigma produced by abstinence campaigns.”
Read more from Yahoo Lifestyle:
‘You won’t live a long life’ and 4 other things people get wrong about this chronic disease
Americans are more obese than ever — and exercise isn’t helping
Follow us on Instagram, Facebook, and Twitter for nonstop inspiration delivered fresh to your feed, every day.

